Abstract
This study aimed to develop a novel virtual reality (VR)-based binocular single vision (BSV) testing system for the quantitative assessment of diplopia and to evaluate its diagnostic accuracy and stability through clinical research. We first developed a VR-based BSV testing apparatus (VR-BSVT) using Oculus Quest 2 VR glasses and Unity software. The system provides three parameters for assessing subjects’ binocular single vision function, and hence their diplopia: VR-BSVF (Virtual Reality-Based Binocular Single Vision Field area), VR-BSVD (Virtual Reality-Based Binocular Single Vision Distance), and VR-BAR (Virtual Reality-Based Binocular Single Vision Field area ratio). Subsequently, we conducted a clinical control study to systematically evaluate the accuracy and stability of VR-BSVT in the quantitative assessment of diplopia. In this comparative study, we recruited 31 visually healthy subjects and 35 patients diagnosed with diplopia. Each participant underwent two VR-BSVT assessments. The diagnostic accuracy of VR-BSVT in identifying diplopia was analyzed using receiver operating characteristic (ROC) curves, Spearman’s rank correlation coefficient, and Bland-Altman analyses. Intraclass correlation coefficient (ICC) was employed to measure the diagnostic stability of VR-BSVT. Through human-computer interaction, VR-BSVT could rapidly detect diplopia and assess binocular single vision function, allowing for the detection of diplopia at different test distances. Among the 66 individuals who participated in the study, results from Intraclass correlation coefficient (ICC) for different test distances showed no significant differences in VR-BAR measurements at both near and far distances between healthy volunteers and patients with diplopia (P = 0.988), indicating good stability of VR-BSVT in diagnosing diplopia. Additionally, the VR-BSVF and VR-BSVD metrics were significantly reduced in the diplopia group compared to the healthy controls (P < 0.01). ROC analysis indicated that VR-BSVT could accurately discriminate patients with diplopia.The Bland-Altman plot revealed a 95% agreement range spanning from − 17.70 to 22.86. These results suggest that VR-BSVT has good precision in diagnosing diplopia. The VR-BSVT developed in this study achieves rapid, accurate, and stable detection and assessment of clinical diplopia, and utilizes virtual reality technology to detect diplopia over a larger visual space. With its compactness and portability, VR-BSVT holds promise for facilitating home healthcare and telemedicine in the future.
Similar content being viewed by others

Introduction
Diplopia is a perceptual abnormality characterized by the simultaneous visualization of a single object as double images within the visual system. This anomaly occurs when the visual system fails to align and integrate the retinal projections from each eye, inhibiting the fusion of these images into a coherent perception. The etiology of diplopia is multifaceted, encompassing neurological disorders, extraocular muscle dysfunction, and strabismus1. Consequently, the resultant asynchrony of binocular visual input not only impairs stereopsis but also diminishes depth perception, significantly hindering routine activities such as balance maintenance, walking, and ocular-centric tasks like reading. In contrast, binocular single vision (BSV) refers to the central integration of corresponding retinal images from both eyes in the visual cortex, with the binocular single vision field (BSVF) defining the spatial extent of this integrative capacity. A reduction in BSVF typically characterizes the clinical manifestations of diplopia and is accompanied by functional impairments that affect daily life2. Given that diplopia can disrupt important daily activities, prompt diagnosis and treatment interventions are imperative.
The quantification of diplopia constitutes a pivotal element in clinical practice, offering profound insights into the severity of the condition, the trajectory of recovery, and the efficacy of therapeutic interventions3. Conventional methods for assessing diplopia involve tools such as the Goldmann perimeter, Hess screen examination4,5,6 and evaluations of cervical range of motion (CROM)7,8, which enable the measurement of diplopia within a predefined field. These techniques facilitate longitudinal monitoring of patients’ progress by tracking the evolution or deterioration of diplopia over time5. However, due to differences in the design principles of these testing devices and interference during the testing process from various factors such as operator disparities and patient cooperation levels, test results may have certain limitations. For instance, the Goldmann perimeter can only measure the binocular single vision field at a distance of 0.33 m in front of the subject’s eyes and is unable to assess the severity of diplopia at longer distances.
In recent years, Virtual Reality (VR) technology has shown rapid development momentum in numerous fields and has been widely applied in visual research9,10. With the aid of VR technology, researchers can construct highly realistic and immersive interactive environments, providing users with unprecedented experiences11. Over the past decade, numerous research teams have successfully applied VR technology in ophthalmic clinical testing, achieving remarkable results. For example, Handa et al. developed a three-dimensional VR display system called CyberDome, which performs excellently in measuring angle of strabismus, with an accuracy comparable to that of traditional prism detection techniques12. Additionally, Tsapakis et al.‘s study indicated that VR-based visual field test results are consistent with those obtained using the standard Humphrey visual field analyzer, demonstrating that VR technology can serve as a new tool for visual field assessment13. These findings not only prove the effectiveness of VR technology in screening ophthalmic diseases but also lay the foundation for its further transformation into practical diagnostic devices. Similarly, the introduction of VR technology offers new solutions for quantifying diplopia in clinical settings. By utilizing VR technology, virtual planes can be directly set at multiple distances in front of the subject’s field of view, enabling long-distance diplopia detection. Moreover, with the help of built-in gyroscope sensors in VR glasses, precise capture of the subject’s head movements is possible, ensuring that the detection plane remains centered in the field of view and avoiding data errors caused by head position changes. This addresses one of the key issues affecting the reliability of traditional diplopia detection methods. More importantly, this technology enables accurate quantitative analysis of BSV, providing a more precise and objective evaluation of diplopia severity.
This study aims to develop and evaluate a novel Virtual Reality (VR)-based Binocular Single Vision (BSV) Testing (BSVT) system to enhance the precision of diplopia detection and quantification. Furthermore, through a prospective clinical controlled study, we systematically evaluated the accuracy and stability of the VR-BSVT in quantitatively assessing diplopia. Our research results confirm that the VR-BSVT system can effectively quantify the binocular single vision function of subjects and demonstrates excellent discriminatory ability in distinguishing clinical diplopia patients. The VR-BSVT system we developed holds promise as a potential replacement for classical methods of diplopia detection. Additionally, leveraging VR technology, we achieved miniaturization and portability of the diplopia testing device, providing the necessary visual function testing equipment for future telemedicine and home care applications.
Abbreviation | Full English Name | Brief English Explanation |
|---|---|---|
BSV | Binocular Single Vision | The central integration of corresponding retinal images from both eyes within the visual center, representing the normal binocular visual function. |
VR | Virtual Reality | Technology that can construct highly realistic and immersive interactive environments for various applications. |
VR-BSVT | Virtual Reality-Based Binocular Single Vision Testing | A testing system based on virtual reality technology used to evaluate binocular single vision and quantify diplopia. |
BSVF | Binocular Single Vision Field | The spatial extent of the integrative capacity of corresponding retinal images from both eyes in the visual center, related to binocular visual function. |
VR-BSVF | Virtual Reality-Based Binocular Single Vision Field | The area of the binocular single vision field measured in the virtual reality environment, helping to assess binocular vision. |
VR-BSVD | Virtual Reality-Based Binocular Single Vision Distance | The sum of distances from the center of the visual field to the BSV boundary in various directions within the reality setting, reflecting morphology of binocular single vision field . |
VR-BAR | Virtual Reality-Based Binocular Single Vision Field area ratio | A metric calculated by dividing the VR-BSVF of an individual by the mean VR-BSVF of healthy volunteers, used to indicate the binocular single vision function of the subject. |
ROC | Receiver Operating Characteristic | A method used to evaluate the diagnostic efficacy of a test by analyzing the relationship between true positive rate and false positive rate. |
BCVA | Best-Corrected Visual Acuity | The best visual acuity that can be achieved with corrective lenses, indicating the visual function after correction. |
ICC | Intra-class Correlation Coefficient | A statistical measure used to assess the reliability or consistency of measurements within the same group or under repeated measurements. |
CI | Confidence Intervals | A range of values within which the true population parameter is likely to fall with a certain level of confidence. |
CROM | Cervical Range of Motion | The range within which the cervical spine can move, which may have implications for certain ocular examinations or conditions. |
AUC | Area Under the Curve | A metric in ROC analysis that represents the overall diagnostic performance of a test, with larger values indicating better performance. |
LoA | Limits of Agreement | The range within which the agreement between two measurement methods is considered acceptable in Bland-Altman analysis. |
FOV | Field of View | The extent of the observable area that can be seen through a device like VR headset, related to the visual range it can cover. |
Methods
Development of VR-BSVT system
VR-BSVT System Development: For the VR hardware system, after considering factors such as cost and portability, we selected Oculus Quest 2 (Meta Corporation, USA), offering a resolution of 1832 × 1920 pixels per eye at a refresh rate of 90 Hz. This VR headset allows fine adjustment of pupillary distance (ranging from 59 to 69 mm) using additional accessories to align with the actual pupillary distance of the user. The VR environment was constructed using Unity software (version: 2020.3.26f1c1). To minimize the impact of head position on detection and ensure precise testing results, the VR-BSVT system employs relative coordinates, maintaining the virtual images in a fixed position relative to the participant’s head regardless of movement or position changes during testing.
Binocular single vision assessment
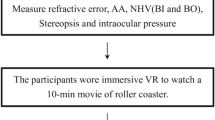
After the start of the test, the VR-BSVT system will display a test plane at different distances ahead of the subject’s field of view (such as 33 cm, 5 m). A green ball is displayed at the center of the test plane, and twelve different orientation test coordinates are displayed around it as shown in Fig. 1. The participants can control the test target along these coordinates using a VR controller and move it toward the periphery of the test plane. When diplopia occurs, i.e., when the green ball turns into two unmerged images, the participants stop moving the test target. At this point, the ___location where the test target is located marks the critical point for binocular single vision. After completing all twelve critical points for diplopia detection, the assessment of binocular single vision is completed. The area formed by these twelve critical points represents the binocular single vision field (BSVF/VR-BSVF, m2). However, to better describe the morphology of VR-BSVF, we measured the distances from each critical point to the center of the test plane and calculated their total sum, which is referred to as VR-BSVD(m). By combining parameters like VR-BSVF and VR-BSVD, we can accurately describe and reflect the range and shape of subjects’ binocular single vision fields. Figure 2 illustrates VR-BSVF measurements for healthy volunteers (a) and patients with diplopia (b). Furthermore, in this study, we defined the ratio of an individual’s VR-BSVF to the mean VR-BSVF area of healthy controls as VR-BAR, as illustrated in the following formula:
Representative schematic of the Virtual Reality-Based Binocular Single Visual Field (VR-BSVF) testing paradigm. The VR-BSVF setup includes two distinct test planes, located at 0.33 m and 5 m from the subject’s ocular axis, respectively. Participants are instructed to fixate on virtual targets. Using a VR controller, participants can manipulate the test target along these coordinates and move it towards the periphery of the test plane. Diplopia occurs when the green ball turns into two unmerged images; at this point, participants stop moving the test target. The ___location where the test target is then indicates the critical point for binocular single vision. After completing all twelve critical points for diplopia detection, the assessment of binocular single vision is complete. The area formed by these twelve critical points represents the binocular single visual field (BSVF/VR-BSVF). Specifically, the maximum BSVF area at a distance of 0.33 m from the participant’s eye axis is approximately 21.3 square meters, while at 5 m, it reaches about 95.5 square meters.
VR-BSVF in healthy volunteers and patients with diplopia. (a) VR-BSVF of healthy volunteers; (b) VR-BSVF of patients with diplopia. VR-BSVF is defined as the area of the irregular polygon enclosed by all identified target positions, whereas VR-BSVD represents the sum of distances from the center point to all identified peripheral target positions, used to describe the morphology of the binocular single visual field.
The VR-BAR indicates the difference between an individual’s binocular single vision function and that of a normal population; a lower VR-BAR value suggests poorer binocular single vision function in the individual.
Participants
This study was a single-center, prospective clinical trial conducted from May to November 2022 at the Second Hospital of Jilin University. We recruited 35 patients with diplopia (24 males and 11 females, with an average age of 40.71 ± 9.90 years) and 31 healthy controls (19 males and 12 females, with an average age of 39.23 ± 11.24 years) for the clinical testing and evaluation of the VR-BSVT system. The study cohort included healthy adults of Asian ethnicity, each having a best-corrected visual acuity (BCVA) of 20/200 (0.1 log MAR) or better in both eyes, and possessing good communication skills and comprehension abilities. Exclusion criteria included individuals with high hyperopia/myopia ( ≥ + 6.0 and − 6.0 diopters sphere), astigmatism ( ≥ + 3.0 and − 3.0 diopters cylinder), or a history of ocular surgery. The study adhered to the principles outlined in the Declaration of Helsinki. Prior to the initiation of the study, written informed consent was obtained from each participant, and the study was approved by the Institutional Review Board of the Second Hospital of Jilin University (Approval No.: 2022 − 145).
The VR-BSVF setup includes two distinct test planes, located at 0.33 m and 5 m from the subject’s ocular axis, respectively. Participants are instructed to fixate on virtual targets. Using a VR controller, participants can manipulate the test target along these coordinates and move it towards the periphery of the test plane. Diplopia occurs when the green ball turns into two unmerged images; at this point, participants stop moving the test target. The ___location where the test target is then indicates the critical point for binocular single vision. After completing all twelve critical points for diplopia detection, the assessment of binocular single vision is complete. The area formed by these twelve critical points represents the binocular single visual field (BSVF/VR-BSVF). Specifically, the maximum BSVF area at a distance of 0.33 m from the participant’s eye axis is approximately 21.3 square meters, while at 5 m, it reaches about 95.5 square meters.
Intergroup Comparison of VR-BSVF and Binocular Range-Based BSVD (BR-BSVD) between Healthy Volunteers and Diplopia Patients. (a) Near vision VR-BSVF comparison between healthy volunteers and diplopia patients. (b) Near vision VR-BSVD comparison between healthy volunteers and diplopia patients. (c) Distant vision VR-BSVF comparison between healthy volunteers and diplopia patients. (d) Distant vision VR-BSVD comparison between healthy volunteers and diplopia patients. (e) ROC curve illustrating the diagnostic efficacy of the diplopia discrimination model employing near and distant vision metrics derived from VR-BSVF and VR-BSVD data. NV: Near Vision; DV: Distant Vision; mean ± S.E.M; ***, P < 0.01.
Clinical examination
All participants underwent a comprehensive medical history assessment to confirm compliance with the inclusion criteria. Additionally, standard ophthalmic examinations, including visual acuity assessments, slit-lamp microscopy, and funduscopy were performed on all subjects. Each participant underwent two VR-BSVT examinations separated by an interval of 15 min during the same visit to ensure consistency in the measurements of VR-BSVF and VR-BSVD.
Statistical analysis
This study utilized IBM SPSS Statistics (Version [X], IBM Corporation, Armonk, New York) for data analysis. Prior to conducting statistical tests, a comprehensive data preparation process was implemented. Outliers were identified using boxplots and Tukey’s fences, ensuring the integrity of the data. The normality of the data distribution was assessed visually through histograms and Q-Q plots, along with the Shapiro-Wilk test. Variables with a p-value greater than 0.05 in the Shapiro-Wilk test were deemed approximately normally distributed. For statistical testing, a chi-square test was used to analyze the differences in sex and age between the diplopia and healthy control groups (since the data were categorical). The intra-class correlation coefficient (ICC) with a 95% confidence interval was employed to measure the agreement of VR-BSVF and VR-BSVD. Receiver operating characteristic (ROC) analysis, with the area under the ROC curve as a key metric, evaluated the diagnostic efficacy of VR-BSVT for detecting diplopia. Spearman’s rank correlation and the Bland-Altman method were utilized to compare BSVF scores and VR-BAR. Finally, differences in VR-BSVF and VR-BSVD between groups were assessed using Student’s t-test for normally distributed data, with a p-value less than 0.05 indicating statistical significance.
Results
Demographic characteristics of the study cohort
Through a meticulous screening and recruitment process, our investigative cohort successfully enrolled 66 participants: 35 patients with diplopia in the diplopia group, and 31 healthy individuals forming the control group. Within the diplopia group, there were 24 males and 11 females. The mean age of the diplopia group was 40.71 ± 9.90 years, with a broad age range spanning from 25 to 67 years, underscoring the diverse representation across different age categories.
The etiologies of diplopia within this group were varied: approximately 16 cases were attributable to orbital wall fractures resulting in restrictive ocular motility disorders; 13 cases stemmed from thyroid-associated ophthalmopathy causing extraocular muscle fibrosis; and an additional 8 cases were due to paralysis of the oculomotor or abducens nerves.
In the control group, there were 19 males and 12 females, with a mean age of 39.23 ± 11.24 years, ranging from 22 to 60 years old. Statistical tests showed no significant differences between the two groups in terms of age (P = 0.569) and gender distribution (P = 0.536), effectively mitigating the interference from demographic imbalances on the interpretation of subsequent findings.
Assessment of stability in diplopia measurements via VR-BSVT
To assess the stability of VR-BSVT test results, we employed the intraclass correlation coefficient (ICC) to evaluate the measuring parameters VR-BSVF and VR-BSVD. As shown in Table 1, the VR-BSVT system demonstrated good reliability for retesting in detecting diplopia. In the proximal diplopia testing plane at 0.33 m, the ICC for VR-BSVF was 0.969 (95% CI = [0.949, 0.981]), while the ICC for VR-BSVD reached 0.974 (95% CI = [0.958, 0.984]). For the distal diplopia testing plane at 5 m, the ICCs for VR-BSVF and VR-BSVD were 0.966 (95% CI = [0.945, 0.979]) and 0.973 (95% CI = [0.957, 0.984]), respectively. These metrics indicate that the VR-BSVT exhibits high stability in detecting diplopia across different distances for both near and far vision tests.
Additionally, we designed the VR-BAR metric, which reflects an individual participant’s VR-BSVF relative to the average VR-BSVF of a healthy volunteer group. As shown in Fig. 3, the VR-BAR for healthy volunteers during near vision tests is 100.01 ± 11.32, and for far vision tests it is 100.00 ± 13.56 (P = 0.988). Similarly, in patients with diplopia, there is no significant difference between the near (49.40 ± 31.12) and far (49.97 ± 32.14) VR-BAR (P = 0.293). By measuring the VR-BAR at both near and far distances, we can assess the stability of the VR-BSVT from another perspective.
Correlational Analysis between VR-BAR and BSVF Scores. Spearman’s rank correlation coefficient along with corresponding P values are indicated on each graph.The dashed line represents the regression line of best fit. (a) All participants; (b) Healthy volunteers; (c) Patients with diplopia; (d) Bland-Altman analysis reveals a high degree of concordance between VR-BAR and BSVF scores.
Assessment of accuracy in diplopia measurements via VR-BSVT
The precision of diplopia measurements utilizing the Virtual Reality Binocular Single Vision Test (VR-BSVT) was assessed by comparing the differences between healthy individuals and those diagnosed with diplopia. As depicted in Fig. 4, the Virtual Reality-Based Binocular Single Visual Field (VR-BSVF) for the control group was recorded as 20.18 ± 2.29 cm² for near vision and 90.44 ± 12.27 m² for far vision. Conversely, the BSVF for patients with diplopia showed a significant reduction to 9.97 ± 6.28 cm² for near distances and 45.20 ± 29.07 m² for far distances (P < 0.001). Additionally, VR-BSVD demonstrated substantial disparities; healthy subjects exhibited values of 284.98 ± 7.70 cm for near distances and 40.63 ± 1.68 m for far distances, while those with diplopia displayed notably lower values of 191.24 ± 76.04 cm and 29.79 ± 11.89 m, respectively (P < 0.001). These findings indicate that both VR-BSVF and VR-BSVD were significantly lower across both near and far visual fields in the diplopia cohort compared to their healthier counterparts. Furthermore, Receiver Operating Characteristic (ROC) analysis confirmed the exceptional diagnostic efficacy of the VR-BSVT in differentiating diplopia. The Area Under the Curve (AUC) values for near and far distances concerning VR-BSVF were 0.9346 (95% CI: [0.8778, 0.9913]) and 0.9161 (95% CI: [0.8496, 0.9827]), respectively. Similarly, the AUCs for VR-BSVD in near and far distances were 0.9650 (95% CI: [0.9108, 1.000]) and 0.9014 (95% CI: [0.8245, 0.9782]), respectively. These results suggest that the VR-BSVT possesses a remarkable capacity to accurately identify individuals afflicted with diplopia.
Additionally, the correlation analysis between VR-BAR and VR-BSVF underscores the diagnostic accuracy of the VR-BSVT for diplopia. As illustrated in Fig. 5, the Spearman’s rank correlation coefficient reveals a strong positive correlation across the entire cohort (r = 0.9368, P < 0.001). This pronounced correlation is also observed within the subset of healthy participants (r = 0.7894, P < 0.001) and is further amplified in the diplopia patient group (r = 0.9463, P < 0.001). The concordance between the two measurement methods was evaluated using the Bland-Altman method. The 95% limits of agreement (LoA) range from − 17.70 to -22.86, indicating substantial agreement between the VR-BAR and VR-BSVF scores in both control and diplopia groups. Notably, there is a subtle trend; the VR-BAR tends to slightly overestimate the VR-BSVF score in healthy volunteers, while it exhibits a slight underestimation trend compared to the VR-BSVF score in patients with diplopia. These findings suggest that the various metrics of the VR-BSVT demonstrate excellent consistency in distinguishing diplopia, highlighting its robust diagnostic accuracy.
Discussion
In this study, we employed virtual reality (VR) technology for the first time in binocular single vision (BSV) assessments to evaluate its efficacy and feasibility in detecting diplopia. Traditional methods of diplopia detection, such as the Goldmann perimeter and Hess screen test, have inherent limitations. These methodologies are typically constrained to a single testing plane and lack the flexibility of multi-plane measurements, thereby failing to comprehensively reflect the true state of binocular single vision. In terms of quantifying diplopia, they offer limited metrics that may not fully capture the complexity of diplopia, potentially leading to less accurate assessments of visual impairment related to binocular vision disorders. In contrast, the VR device utilized in this study exhibits significant advantages in BSV measurement. By leveraging VR technology, the device can assess multiple testing planes, simulate various real-life visual scenarios, and provide a more comprehensive and three-dimensional perspective, thereby enhancing assessment accuracy. When quantifying diplopia, the VR device provides several quantifiable parameters such as VR-BSVF, VR-BSVD, and VR-BAR, reflecting different aspects of the morphology and function of binocular single vision and aiding in a deeper understanding of the severity of diplopia. Combining these parameters allows for a more comprehensive representation of the binocular single vision state, offering richer information for diplopia assessment.
To validate the stability and accuracy of the VR device in diplopia assessment, we conducted a comparative clinical study involving patients with diplopia and healthy volunteers. The results demonstrated that VR-BSVT performed exceptionally well in distinguishing between healthy individuals and those with diplopia, exhibiting high diagnostic performance. Through intraclass correlation coefficient (ICC) analysis, we confirmed the stability of VR-BSVF and VR-BSVD within VR-BSVT when evaluating near and distance diplopia. Additionally, receiver operating characteristic (ROC) curve analysis revealed a significant positive correlation between VR-BAR and BSVF scores, further validating the accuracy of VR-BSVT in diplopia assessment. Notably, VR-BAR is calculated as the ratio of an individual’s VR-BSVF to the average VR-BSVF of healthy controls, resulting in relatively higher VR-BAR values for healthy volunteers. Conversely, patients with diplopia typically exhibit lower VR-BAR values compared to healthy volunteers.
VR-BSVT offers several advantages in the detection and quantification of diplopia. Firstly, it employs human-computer interaction and standardized procedures, reducing test bias and enabling more accurate quantification of the binocular single vision range or the severity of diplopia. Secondly, for patients who are critically ill or severely injured and unable to undergo traditional BSVF scoring, VR-BSVT can be administered bedside, which holds significant clinical relevance. Moreover, target positioning in VR-BSVT is linked to the subject’s head movement, mitigating the impact of gaze deviation and allowing subjects to move their heads freely without interrupting the test, thereby enhancing result reliability. Finally, the testing process does not require face-to-face interaction with the patient, achieving digitalization of traditional BSVF scoring and demonstrating potential applications in telemedicine. Future advancements may enable automatic diplopia measurement without direct assistance from clinicians. However, this study also has certain limitations. Due to the limited field of view (FOV) of the VR headset, the detected binocular single vision range is smaller than the actual human binocular single vision range, but this issue is anticipated to be addressed with ongoing technological advancements. Although all subjects completed the tests under clinical supervision, the possibility of poor compliance cannot be entirely excluded. Furthermore, as a single-center, small sample size study, the calculated normal ranges for VR-BSVF and VR-BSVD may deviate from the true ranges. Future large-sample, multicenter studies are necessary to further validate these findings.
Conclusion
This study designed, implemented, and tested a novel VR-based method for detecting diplopia, further corroborating the utility and feasibility of VR-BSVT in assessing BSV and diplopia. The results demonstrate that VR-BSVT possesses high sensitivity and accuracy in detecting diplopia and distinguishing it from healthy conditions. It can also quantify the severity of diplopia with greater precision. Testing BSVF in a VR environment marks the first crucial step towards digitizing diplopia examination and paves the way for its application in telemedicine. Despite certain limitations, this work suggests that VR technology holds immense potential as an assessment tool for diplopia.
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Yoo, H. S. et al. A computerized red glass test for quantifying diplopia. BMC Ophthalmol. 17 (1), 71 (2017).
Narita, I. et al. Effects of orthoptic training for residual diplopia after surgical repair of blowout fractures. Graefes Arch. Clin. Exp. Ophthalmol. 260 (4), 1395–1404 (2022).
Hatt, S. R., Leske, D. A. & Holmes, J. M. Comparing methods of quantifying diplopia. Ophthalmology 114 (12), 2316–2322 (2007).
Woodruff, G., O’Reilly, C. & Kraft, S. P. Functional scoring of the field of binocular single vision in patients with diplopia. Ophthalmology 94 (12), 1554–1561 (1987).
Fitzsimons, R. & White, J. Functional scoring of the field of binocular single vision. Ophthalmology 97 (1), 33–35 (1990).
Sullivan, T. J. et al. A functional scoring method for the field of binocular single vision. Ophthalmology 99 (4), 575–581 (1992).
Kushner, B. J. The usefulness of the cervical range of motion device in the ocular motility examination. Arch. Ophthalmol. 118 (7), 946–950 (2000).
Holmes, J. M., Leske, D. A. & Kupersmith, M. J. New methods for quantifying diplopia. Ophthalmology 112 (11), 2035–2039 (2005).
Yeh, P. H. et al. To measure the amount of ocular deviation in strabismus patients with an eye-tracking virtual reality headset. BMC Ophthalmol. 21 (1), 246 (2021).
Tseng, R. et al. Emergence of non-artificial intelligence digital health innovations in ophthalmology: A systematic review. Clin. Exp. Ophthalmol. 49 (7), 741–756 (2021).
Ma, M. K. I. et al. Virtual reality and augmented reality- emerging screening and diagnostic techniques in ophthalmology: A systematic review. Surv. Ophthalmol. 67 (5), 1516–1530 (2022).
Handa, T. et al. A novel apparatus for testing binocular function using the ‘cyberdome’ three-dimensional hemispherical visual display system. Eye (Lond). 23 (11), 2094–2098 (2009).
Tsapakis, S. et al. Visual field examination method using virtual reality glasses compared with the Humphrey perimeter. Clin. Ophthalmol. 11, 1431–1443 (2017).
Funding
The study was funded by the Jilin Province Special Project for Talent in Medical and Health Sciences (No.2024WSXK-E01) and Jilin University’s Program for Validating Scientific and Technological Concepts (No.23NYZ05).
Author information
Authors and Affiliations
Contributions
B Y: Conceptualization, Methodology, Investigation; YH. L,YL.L and MY. W: VR System developing; GY. L: Conceptualization, Writing – original draft, Writing – review & editing, Funding acquisition, Resources, Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yu, B., Li, YH., Li, YL. et al. Enhanced diplopia detection and binocular single vision assessment through virtual reality: A comprehensive study. Sci Rep 15, 8355 (2025). https://doi.org/10.1038/s41598-025-92996-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92996-5