Abstract
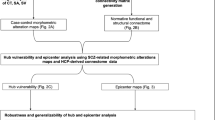
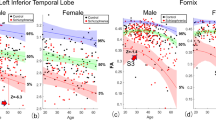
Understanding the neuroanatomy of schizophrenia remains elusive due to heterogeneous findings across neuroimaging studies. Here we investigated whether patterns of brain atrophy associated with schizophrenia would localize to a common brain network using a coordinate network mapping meta-analysis approach. Utilizing the human connectome as a wiring diagram, we identified a connectivity pattern, a schizophrenia network, uniting heterogeneous results from 90 published studies of atrophy in schizophrenia (total n > 8,000). This network was specific to schizophrenia, differentiating it from atrophy in individuals at high risk for psychosis (n = 3,038), normal aging (n = 4,195), neurodegenerative disorders (n = 3,707) and other psychiatric conditions (n = 3,432). The network was also stable with disease progression and across different clusters of schizophrenia symptoms. Patterns of brain atrophy in schizophrenia were negatively correlated with lesions linked to psychosis-related thought processes in an independent cohort (n = 181). Our results propose a unique, stable, and unified schizophrenia network, addressing a significant portion of the heterogeneity observed in previous atrophy studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
79,00 € per year
only 6,58 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All atrophy coordinates used in this work are derived from previously published studies, as referenced in previous meta-analyses23,49,50. The functional connectivity data utilized in this study can be accessed online through the Harvard Dataverse at https://doi.org/10.7910/DVN/ILXIKS. For inquiries related to the Vietnam Head Injury Study, please contact J. Grafman at [email protected]. The final schizophrenia network map is available via NeuroVault (https://neurovault.org/images/889224/).
Code availability
The processing pipeline for functional connectivity data can be found at https://github.com/bchcohenlab/BIDS_to_CBIG_fMRI_Preproc2016. The statistical analyses were conducted using MATLAB R2022b. MATLAB code for spatial permutation testing can be accessed via Zenodo at https://zenodo.org/records/13851081 (ref. 54).
References
Vigo, D., Thornicroft, G. & Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry. 3, 171–178 (2016).
Keshavan, M. S. et al. Neuroimaging in schizophrenia. Neuroimaging Clin. N. Am. 30, 73–83 (2020).
Kraguljac, N. V. & Lahti, A. C. Neuroimaging as a window into the pathophysiological mechanisms of schizophrenia. Front. Psychiatry. 12, 613764 (2021).
Dabiri, M. et al. Neuroimaging in schizophrenia: a review article. Front. Neurosci. 16, 1042814 (2022).
Ortiz-Gil, J. et al. Neural correlates of cognitive impairment in schizophrenia. Br. J. Psychiatry. 199, 202–210 (2011).
Pomarol-Clotet, E. et al. Medial prefrontal cortex pathology in schizophrenia as revealed by convergent findings from multimodal imaging. Mol. Psychiatry 15, 823–830 (2010).
Chang, M. et al. Correction: voxel-based morphometry in individuals at genetic high risk for schizophrenia and patients with schizophrenia during their first episode of psychosis. PLoS ONE. 12, e0170146 (2017).
Delvecchio, G. et al. Brain anatomy of symptom stratification in schizophrenia: a voxel-based morphometry study. Nord. J. Psychiatry. 71, 348–354 (2017).
Huang, P. et al. Decreased bilateral thalamic gray matter volume in first-episode schizophrenia with prominent hallucinatory symptoms: a volumetric MRI study. Sci. Rep. 5, 14505 (2015).
Hu, M. L. et al. A review of the functional and anatomical default mode network in schizophrenia. Neurosci. Bull. 33, 73–84 (2017).
Menon, V., Palaniyappan, L. & Supekar, K. Integrative brain network and salience models of psychopathology and cognitive dysfunction in schizophrenia. Biol. Psychiatry 94, 108–120 (2023).
van Erp, T. G. M. et al. Cortical brain abnormalities in 4474 individuals with schizophrenia and 5098 control subjects via the Enhancing Neuro Imaging Genetics Through Meta Analysis (ENIGMA) Consortium. Biol. Psychiatry 84, 644–654 (2018).
van Erp, T. G. et al. Subcortical brain volume abnormalities in 2028 individuals with schizophrenia and 2540 healthy controls via the ENIGMA consortium. Mol. Psychiatry 21, 585 (2016).
Cash, R. F. H., Müller, V. I., Fitzgerald, P. B., Eickhoff, S. B. & Zalesky, A. Altered brain activity in unipolar depression unveiled using connectomics. Nat. Ment. Health. 1, 174–185 (2023).
Siddiqi, S. H., Khosravani, S., Rolston, J. D. & Fox, M. D. The future of brain circuit-targeted therapeutics. Neuropsychopharmacology 49, 179–188 (2023).
Darby, R. R., Joutsa, J. & Fox, M. D. Network localization of heterogeneous neuroimaging findings. Brain 142, 70–79 (2019).
Zhukovsky, P. et al. Coordinate-based network mapping of brain structure in major depressive disorder in younger and older adults: a systematic review and meta-analysis. Am. J. Psychiatry. 178, 1119–1128 (2021).
Stubbs et al. Heterogeneous neuroimaging findings across substance use disorders localize to a common brain network. Nat. Ment. Health. 1, 772–781 (2023).
Weil, R. S., Hsu, J. K., Darby, R. R., Soussand, L. & Fox, M. D. Neuroimaging in Parkinson’s disease dementia: connecting the dots. Brain Commun. 1, fcz006 (2019).
Burke, M. J. et al. Mapping migraine to a common brain network. Brain 143, 541–553 (2020).
Taylor, J. J. et al. A transdiagnostic network for psychiatric illness derived from atrophy and lesions. Nat. Hum. Behav. 7, 420–429 (2023).
Eickhoff, S. B., Bzdok, D., Laird, A. R., Kurth, F. & Fox, P. T. Activation likelihood estimation meta-analysis revisited. Neuroimage 59, 2349–2361 (2012).
Liloia, D. et al. Updating and characterizing neuroanatomical markers in high-risk subjects, recently diagnosed and chronic patients with schizophrenia: a revised coordinate-based meta-analysis. Neurosci. Biobehav. Rev. 123, 83–103 (2021).
Yeo, B. T. et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol. 106, 1125–1165 (2011).
Dice, L. R. Measures of the amount of ecologic association between species. Ecology 26, 297–302 (1945).
Siddiqi, S. H. et al. Brain stimulation and brain lesions converge on common causal circuits in neuropsychiatric disease. Nat. Hum. Behav. 5, 1707–1716 (2021).
Yarkoni, T., Poldrack, R. A., Nichols, T. E., Van Essen, D. C. & Wager, T. D. Large-scale automated synthesis of human functional neuroimaging data. Nat. Methods 8, 665–670 (2011).
Siddiqi, S. H., Kording, K. P., Parvizi, J. & Fox, M. D. Causal mapping of human brain function. Nat. Rev. Neurosci. 23, 361–375 (2022).
Raymont, V., Salazar, A. M., Krueger, F. & Grafman, J. “Studying injured minds”—the Vietnam Head Injury Study and 40 years of brain injury research. Front. Neurol. 2, 15 (2011).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 4th edn (American Psychiatric Association, 1994).
Arkin, S. C. et al. Deficits and compensation: attentional control cortical networks in schizophrenia. Neuroimage Clin. 27, 102348 (2020).
Jimenez, A. M. et al. Abnormal ventral and dorsal attention network activity during single and dual target detection in schizophrenia. Front. Psychol. 7, 323 (2016).
Keyvanfard, F., Schmid, A. K. & Nasiraei-Moghaddam, A. Functional connectivity alterations of within and between networks in schizophrenia: A retrospective study. Basic Clin. Neurosci. 14, 397–409 (2023).
Sheffield, J. M. & Barch, D. M. Cognition and resting-state functional connectivity in schizophrenia. Neurosci. Biobehav. Rev. 61, 108–120 (2016).
van den Heuvel, M. P. & Fornito, A. Brain networks in schizophrenia. Neuropsychol. Rev. 24, 32–48 (2014).
Dong, D. et al. Shared abnormality of white matter integrity in schizophrenia and bipolar disorder: a comparative voxel-based meta-analysis. Schizophr. Res. 185, 41–50 (2017).
Kim, N. Y. et al. Lesions causing hallucinations localize to one common brain network. Mol. Psychiatry 26, 1299–1309 (2021).
Darby, R. R., Laganiere, S., Pascual-Leone, A., Prasad, S. & Fox, M. D. Finding the imposter: brain connectivity of lesions causing delusional misidentifications. Brain 140, 497–507 (2017).
Kraepelin, E. Dementia Praecox and Paraphrenia (Chicago Medical Book Co., 1919).
Silbersweig, D. & Loscalzo, J. Precision psychiatry meets network medicine: network psychiatry. JAMA Psychiatry 74, 665–666 (2017).
Wood, S. J. et al. Progressive changes in the development toward schizophrenia: studies in subjects at increased symptomatic risk. Schizophr. Bull. 34, 322–329 (2008).
Collins, M. A. et al. Accelerated cortical thinning precedes and predicts conversion to psychosis: the NAPLS3 longitudinal study of youth at clinical high-risk. Mol. Psychiatry 28, 1182–1189 (2023).
Fornito, A. et al. Anatomic abnormalities of the anterior cingulate cortex before psychosis onset: an MRI study of ultra-high-risk individuals. Biol. Psychiatry 64, 758–765 (2008).
Takayanagi, Y. et al. Reduced thickness of the anterior cingulate cortex in individuals with an at-risk mental state who later develop psychosis. Schizophr. Bull. 43, 907–913 (2017).
Galovic, M. et al. Progressive cortical thinning in patients with focal epilepsy. JAMA Neurol. 76, 1230–1239 (2019).
Lacadie, C. M., Fulbright, R. K., Rajeevan, N., Constable, R. T. & Papademetris, X. More accurate Talairach coordinates for neuroimaging using non-linear registration. Neuroimage. 42, 717–725 (2008).
Winkler, A. M., Ridgway, G. R., Webster, M. A., Smith, S. M. & Nichols, T. E. Permutation inference for the general linear model. Neuroimage 92, 381–397 (2014).
Smith, S. M. & Nichols, T. E. Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage 44, 83–98 (2009).
Goodkind, M. et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry 72, 305–315 (2015).
Minkova, L. et al. Gray matter asymmetries in aging and neurodegeneration: a review and meta-analysis. Hum. Brain. Mapp. 38, 5890–5904 (2017).
The MathWorks Inc. MATLAB version: 9.13.0 (R2022b) https://www.mathworks.com (2022).
Weinstein, S. M. et al. A simple permutation-based test of intermodal correspondence. Hum. Brain. Mapp. 42, 5175–5187 (2021).
Siddiqi, S. H. et al. Lesion network localization of depression in multiple sclerosis. Nat. Ment. Health 1, 36–44 (2023b).
Makhlouf, A. & Siddiqi, S. Heterogenous patterns of brain atrophy in schizophrenia localize to a common brain network. Zenodo https://zenodo.org/records/13851081 (2024).
Acknowledgments
We express our gratitude to the participants who volunteered for the studies analyzed in this paper. We thank A. Cohen, M. Ferguson, C. Lin, and L. Soussand for their efforts in developing the computational methods used in this study. We also thank P. Flynn and L. Sterina for administrative support. This work was supported by the following sources: Harvard Medical School (Dupont Warren Fellowship Award) and the NIH (grant no. R01MH113929) (A.T.M.); Canadian Institutes of Health Research Vanier Scholarship and a University of British Columbia Friedman Award for Scholars in Health (J.L.S.); Harvard Medical School (Dupont Warren Fellowship Award and Livingston Award), Brain and Behavior Research Foundation Young Investigator Grant (no. 31081), Sidney R. Baer, Jr. Foundation, Baszucki Brain Research Fund, and the NIH (grant nos K23MH129829 and R01MH113929) (J.J.T.); the Nancy Lurie Marks Foundation, the Kaye Family Research Endowment, the Baszucki Brain Research Fund and the NIH (grant nos. R01MH113929, R21MH126271, R56AG069086, R01MH115949, and R01AG060987) (M.D.F.); the NIH (grant nos. K23MH121657, R21MH126271, and R01MH136248), the Brain and Behavior Research Foundation Young Investigator Grant, the Baszucki Brain Research Fund and the Department of Veterans Affairs (grant no. I01CX002293) (S.H.S.).
Author information
Authors and Affiliations
Contributions
A.T.M., D.S., M.D.F., and S.H.S. conceived and designed the study. A.T.M., W.D., J.L.S., M.D.F., and S.H.S. designed the analytical procedures. A.T.M., W.D., J.L.S., J.J.T., and D.L. preprocessed and prepared the data for analysis. A.T.M., W.D., J.L.S., J.J.T., and S.H.S. performed the neuroimaging and statistical analyses. D.L., J.J.T., J.L.S., and J.G. contributed the data. A.T.M. and S.H.S. wrote the paper, with input from all authors.
Corresponding author
Ethics declarations
Competing interests
S.H.S. holds intellectual property related to using individualized resting-state network mapping for targeting TMS, filed in 2016, which has not generated royalties and is unrelated to this work. S.H.S. also serves as a scientific consultant for Magnus Medical, has received investigator-initiated research funding from Neuronetics (2019) and Brainsway (2022), received speaking fees from Brainsway (2021) and Otsuka (for PsychU.org, 2021) and holds shares in Brainsway (publicly traded) and Magnus Medical (privately held). M.D.F. is a scientific consultant for Magnus Medical and owns separate intellectual property related to using functional connectivity to target TMS for depression, filed in 2013, which has not generated royalties and is unrelated to this work. The other authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Richard Dear, Golia Shafiei, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–12, Tables 1–7, and References.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Makhlouf, A.T., Drew, W., Stubbs, J.L. et al. Heterogeneous patterns of brain atrophy in schizophrenia localize to a common brain network. Nat. Mental Health 3, 19–30 (2025). https://doi.org/10.1038/s44220-024-00348-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-024-00348-5
This article is cited by
-
Distinct structural deficits in treatment-resistant schizophrenia and their putative neurotransmitter basis: a source-based morphometry analysis
Neuropsychopharmacology (2025)
-
Heterogeneous patterns of brain atrophy in schizophrenia localize to a common brain network
Nature Mental Health (2024)