Abstract
Aim:
It is unclear why α1D-adrenergic receptors (α1D-ARs) play a critical role in the mediation of peripheral vascular resistance and blood pressure in situ but function inefficiently when studied in vitro. The present study examined the causes for these inconsistencies in native α1-adrenergic functional performance between the vascular smooth muscle and myocytes.
Methods:
The α1-adrenergic mediated contraction, Ca2+ signaling and the subcellular receptor distribution were evaluated using the Fluo-4, BODIPY-FL prazosin and subtype-specific antibodies.
Results:
Rat aortic rings and freshly dissociated myocytes displayed contractile and increased intracellular Ca2+ responses to stimulation with phenylephrine (PE, 10 μmol), respectively. However, the PE-induced responses disappeared completely in cultured aortic myocytes, whereas PE-enhanced Ca2+ transients were seen in cultured rat cardiac myocytes. Further studies indicated that α1D-ARs, the major receptor subtype responsible for the α1-adrenergic regulation of aortic contraction, were distributed both intracellularly and at the cell membrane in freshly dispersed aortic myocytes, similar to the α1A-AR subcellular localization in the cultured cardiomyocytes. In the cultured aortic myocytes, however, in addition to a marked decrease in their protein expression relative to the aorta, most labeling signals for α1D-ARs were found in the cytoplasm. Importantly, treating the culture medium with charcoal/dextran caused the reappearance of α1D-ARs at the cell surface and a partial restoration of the Ca2+ signal response to PE in approximately 30% of the cultured cells.
Conclusion:
Reduction in α1D-AR total protein expression and disappearance from the cell surface contribute to the insensitivity of cultured vascular smooth muscle cells to α1-adrenergic receptor activation.
Similar content being viewed by others
Introduction
The activation of α1-adrenergic receptors (α1ARs) and their downstream intracellular signal transduction pathways is a key event for the regulation of arterial contractility and control of blood pressure by the sympathetic nervous system. α1ARs are members of the Gq protein-coupled receptor (GPCR) superfamily that, upon stimulation, activate phospholipase C and catalyze the cleavage of polyphosphoinositide into dual signaling molecules, inositol 1,4,5-trisphosphate (IP3) and diacylglycerol1, 2. The IP3 formation leads to the mobilization of intracellular Ca2+ stores and, in combination with Ca2+ influx across the plasma membrane, eventually initiates arterial vasoconstriction2, 3. On the other hand, diacylglycerol enables protein kinase C to phosphorylate target proteins and modulate multiple cellular processes1, 2, 3, 4.
Pharmacological and gene encoding analyses have identified that the α1AR family has three subtypes: α1A-ARs, α1B-ARs, and α1D-ARs2, 5. Although all three subtypes are coupled to GPCR, they differ in their tissue distributions, affinities to ligands, and apparent efficiencies for intracellular couplings6, 7. To date, the clearest differences among the α1AR subtypes are in their subcellular localizations: α1A-ARs and α1B-ARs are primarily located at the plasma membrane while the majority of α1D-ARs are found accumulated within the intracellular compartments of both recombinant and native cells7, 8, 9, 10. Additionally, divergent factors or mechanisms have been found to differentially regulate the subtypes in regards of the receptor internalization/trafficking recycling, expression, and sensitivity of the signaling and effector molecules that they are coupling, rendering a fine tuning for the α1-adrenergic responsiveness to different biological signals and for adapting cells to changes in the internal milieu and to overall homeostasis2, 6, 10, 11, 12. Therefore, exploring the receptor characteristics of and regulatory mechanisms for each subtype is important for understanding and explicating their functional roles in both physiological and pathophysiological processes.
An increasing number of studies in vivo as well as in vitro have been performed to examine the cellular functions and regulatory mechanisms of α1A-ARs and α1B-ARs2, 6, 10, 11, 12. Also, α1D-ARs have been found to mediate contractile responses to catecholamines in several blood vessels with high potency13, 14. In addition, they are thought to be the critical mediator of normal blood pressure15, 16 and hypertension related to aging17, high salt hypertension18 and spontaneous hypertension19 in situ. However, unlike the situation for α1A- and α1B-ARs, information regarding α1D-AR cellular functions and their underlying regulatory mechanisms is scant because of the difficulties in obtaining sufficient function in native or recombinant cells in vitro, raising the question of whether manifestations of the α1D-ARs expressed in vitro are, in fact, representative of the physiological situation9, 11, 12. In the current study, we sought to determine the causes for the inconsistencies in α1AR regulatory effects on vascular contractility between the in vivo and in vitro studies by comparing α1AR-mediated Ca2+ signaling and its subcellular distribution in native rat aortic and cardiac myocytes (α1D-AR and α1A-AR subtypes are known to contribute mainly to α1 adrenergic mediation of constriction in the rat aorta13, 14 and cardiac muscle20, 21, 22, 23, 24, respectively).
Materials and methods
Materials
All reagents and drugs used were purchased from Sigma, except A61603 (N-[5-(4,5-dihydro-1H-imidazol-2yl)-2-hydroxy-5,6,7,8-tetrahydronaphthalene-1-yl]methanesulfonamide hydrobromide) and Fluo-4/AM, which were obtained from Tocris (Ellisville, MO, USA) and Molecular Probes, respectively.
Measurement of aortic contraction
Male Sprague-Dawley rats (220±20 g) and ICR mice (20±2 g) were used and handled in accordance with the Guide for Care and Use of Laboratory Animals published by the Beijing Municipal Government. Animals were sacrificed by the administration of a rapid intraperitoneal injection of pentobarbital sodium (100 mg/kg). Vessel preparation and the preparation of HEPES-buffered saline solution (HBSS) have been described previously25, 26. Briefly, an approximately 15 mm (rat) or 8 mm (mice) portion of the descending thoracic aorta was excised, and the endothelium was removed by rubbing the luminal surface. Aortic rings 2−3 mm in width were prepared and mounted into one of eight organ baths containing 20 mL HBSS gassed with 100% O2 at 37 °C. The rings were equilibrated under 0.5 or 1.0 g of passive tension (for the mouse or rat aorta, respectively) for 1.5 h, and their isometric force was measured with a force-displacement transducer connected to a carrier amplifier and analyzed with AcqKnowledge software (MP150, Biopac Systems, Inc).
Isolation and culture of aortic vascular smooth muscle cells
Isolation and culture of vascular smooth muscle cells (VSMCs) from the mouse aorta have been described previously26. Rat thoracic aortic myocytes were isolated as follows. Adipose and connective tissues, as well as endothelial cells, were removed, and aortas were digested in HBSS containing 1 mg/mL collagenase (type II, Worthington Biochem), 0.2 mg/mL elastase (type III, Sigma), and 1 mg/mL bovine serum albumin for 20 min at 37 °C. Following incubation, the aortas were massaged and flushed with HBSS. The dissociated VSMCs were collected by centrifugation and either seeded onto laminin-coated dishes for measurements of intracellular Ca2+ concentration ([Ca2+]i) in freshly isolated cells or plated into plastic tissue culture dishes and grown in Dulbecco's modified Eagle's medium (DMEM, Hyclone) containing 10% fetal bovine serum, 4 mmol L-glutamine, 100 U/mL penicillin and 100 μg/mL streptomycin (Hyclone) at 37 °C under 5% CO2–95% air. Cells were used from the third through the eighth passages.
Measurement of intracellular Ca2+
The aortic VSMCs from rats or mice were loaded with 4 μmol Fluo-4/AM in DMEM at 37 °C for 30 min and washed three times with HBSS for 20 min. [Ca2+]i was then measured as described previously21.
Immunocytochemistry
VSMCs were fixed in 4% formaldehyde in phosphate-buffered saline (PBS) for 10 min, permeabilized with 0.1% Triton X-100, and then blocked in PBS containing 5% bovine serum albumin, 5% horse serum and 0.05% Triton X-100 for 1 h. Antibodies specific for α1A-ARs or α1D-ARs were added and incubated overnight at 4 °C at a dilution of 1:100 (Santa Cruz). Secondary antibodies used were Alexa Fluor 594 chicken anti-goat or Alexa Fluor 488 goat anti-rabbit (Invitrogen) at a dilution of 1:500. For the binding measurement of BODIPY FL prazosin, living myocytes were washed twice with HBSS, loaded with HBSS containing 2 μmol BODIPY FL prazosin, 1% bovine serum albumin and 0.1% F127 for 30 min at room temperature. Analysis of subcellular immunostaining was performed using a Leica SP 5 confocal microscope equipped with a 40x oil immersion objective lens (NA 1.25).
Immunoblotting
Rat aortic smooth muscle and cultured myocytes were lysed in RIPA buffer containing 1 mmol polymethylsulfonyl fluoride and 2 μg/mL protease inhibitor cocktail (Santa Cruz) for 1 h on ice. Homogenates were centrifuged for 15 min at 14 000×g at 4 °C. Lysates of 30 μg in cells or 15 μg in tissue were heated for 5 min, resolved on a 10% SDS-PAGE gel and transferred to PVDF membrane. Membranes were blocked with 5% nonfat milk powder in Tris-buffered saline containing 0.1% (v/v) Tween 20 for 60 min at room temperature and then probed with specific antibodies against α1A- or α1D-ARs at a dilution of 1:500 overnight at 4 °C. The immunoblotted membrane was then incubated with horseradish peroxidase-conjugated secondary antibody for 1 h, and immunoreactive bands were detected using an enhanced chemiluminescence kit (ECL-plus).
Statistical analysis and data presentation
Mechanical responses of the arteries were expressed as the increase in force (g). All results are reported as means±SEM (n=number of cells or arteries, as indicated). Statistical differences between means were analyzed using a two-way paired or unpaired Student's t-test or χ2 test, when appropriate. Probability levels <5% were considered significant.
Results
Contractile and internal Ca2+ signal responses of rat and mouse aortas to α1AR activation
To investigate the native α1AR function at the tissue level, the non-subtype selective α1AR agonist phenylephrine (PE)-induced vasoconstriction was evaluated in rat aortic rings. Similar to the response induced by 80 mmol KCl depolarization, PE (10 μmol) evoked a strong tonic constriction in the vessels, which was completely abolished by prazosin, a specific antagonist for α1ARs (Figure 1A). In a Ca2+-free medium, a transient contractile response to PE was followed by a relaxation to the baseline level, suggesting an internal Ca2+ release-related constriction. Upon the re-addition of extracellular CaCl2 (2.0 mmol) in the presence of PE, further sustained force was induced (Figure 1B). This force could be decreased significantly by nifedipine (1 μmol, data not shown), demonstrating an extracellular Ca2+-dependent constriction of this part. Additionally, as a reference for vasoconstriction regulation among GPCR members, angiotensin II (Ang II), an agonist of the angiotensin receptor, was also examined in this study; Ang II produced similar responses to PE in the rings (Figure 1B). Therefore, these data demonstrate a common characteristic of Ca2+-dependent vasoconstriction by the activation of two different GPCR members, consistent with previous studies on arteries25, 27, 28.
Differences in contractile and intracellular Ca2+ signal responses to α1-adrenergic receptor activation between the rat thoracic aorta and cultured aortic smooth muscle cells. (A) Stimulating rat aortic rings with PE or high KCl concentration (80 mmol) (indicated with an arrow) induced a tonic force in Ca2+ containing HBSS. Pretreatment of the rings with 1 μmol prazosin for 10 min abolished the effect of PE, but not that of high KCl. (B) PE or Ang II caused a transient aortic contraction in Ca2+-free medium, followed by a tonic constriction upon Ca2+ addition to the medium. (C and D) A [Ca2+]i increase upon stimulation with high KCl (C) or Ang II (D), but not with PE, in cultured aortic VSMCs loaded with fluo4. Numbers for each curve in all panels ranged from 6 to 12 separate experiments.
To investigate the native α1AR function at the cellular level, α1AR-mediated [Ca2+]i signaling was further measured in isolated aortic VSMCs by confocal microscopy. Unlike in rat aortic rings, the cultured VSMCs did not respond to PE (10 to 300 μmol), but exhibited a striking [Ca2+]i increase to the addition of 40 mmol KCl and stimulation with Ang II (Figures 1C and D). This observation was generally identical in the third to eighth cultured VSMCs passages and also in all passages of A7R5 cells (a cell line of rat aorta, data not shown), suggesting that a similar phenomenon occurs in different culture of cells.
Since the α1D-AR subtype is tightly linked to blood pressure control in mice15, 16, we also investigated the α1AR-mediated Ca2+ signaling responses in vessels and VSMCs in mice. ATP, an activator of the purinic receptor (a member of GPCR superfamily)26, was used for comparison, because Ang II was unable to cause observable vasoconstriction in the mouse thoracic aorta. Similar to the situation in rats, PE caused a remarkable aortic contraction in mouse aorta, but failed to induce any Ca2+ signal response in the cultured VSMCs, whereas ATP elicited a relatively weak tension in the vessel and a profound rise in [Ca2+]i in cultured mouse VSMCs (Figures 2A and B). This much weaker aorta contraction induced by ATP than by the other GPCR receptor activators is likely due to ATP's additional relaxing effect on vessels caused by activation of protein kinase A29 and the delayed ATP-elicited potassium channel30.
Differences in contractile and intracellular Ca2+ signal responses to α1-adrenergic receptor activation between mouse thoracic aorta and cultured aortic smooth muscle cells. (A) Stimulating the mouse aortic rings with PE or ATP (indicated with an arrow) caused a sustained or somewhat weak constriction in Ca2+-containing medium, respectively. (B) In Fluo-4-loaded cultured mouse VSMCs, ATP, but not PE, was able to induce an increase in [Ca2+]i. Numbers for each curve were from 5 to 7 separate experiments.
Intracellular Ca2+ signal responses to α1AR activation in freshly isolated thoracic aortic myocytes
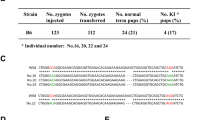
The above results indicate that among the three members of the GPCR family, only the α1AR-coupled Ca2+ signaling pathway in the vessels was somehow masked in the culture condition, implying some alteration in the α1AR themselves occurred during the cell dissociation or/and culturing procedures. Thus, we further examined the α1AR-mediated Ca2+ signals in rat aortic myocytes of freshly isolated, and primarily cultured for <1 day, ≥2 days or beyond 3 days. VSMCs were identified morphologically and functionally by their ability to respond to 40 mmol KCl by contracting and [Ca2+]i increasing. Cells that did not exhibit a Ca2+ response to high K+ depolarization were not used. As shown in Figure 3 and Table 1, PE induced an obvious cell shortening and simultaneous [Ca2+]i increase in 91.6±4.3% of freshly dispersed and 55.2±4.9% of cultured <1 day VSMCs (n=32 and 40, respectively), but completely failed to evoke any [Ca2+]i response in the cells cultured for 2 days or beyond, all of which remained responsive ability to either high K+ or Ang II stimulation. Therefore, the results indicate that the α1AR-coupled Ca2+ signaling pathway in VSMCs is gradually and ultimately blocked by cell culture, not cell isolation.
Contractile and intracellular Ca2+ signal responses to α1-adrenergic activation in freshly dissociated rat aortic smooth muscle cells. Two typical cells represent PE-induced cell shortening (images of cell one, upper panel) and simultaneous [Ca2+]i increases (traces for the two cells, bottom panel) in partial freshly dispersed or cultured <1 day aortic myocytes, with high KCl induced responses in all myocytes tested. The summarized data for PE, high KCl and Ang II are described in Table 1.
Intracellular Ca2+ signal responses to α1AR activation in primary cultured cardiac ventricular myocytes
Unlike in the VSMCs, functional α1AR-mediated Ca2+ signals, such as increasing [Ca2+]i or spontaneous Ca2+ transient rate have been shown in primary cultured neonatal mouse or rat ventricular myocytes (NRVM)21, 22, 23, 24, implying unaltered responsibility for cardiomyocytes to α1AR activation even in the culture state. To clarify this, we testified the PE effect on [Ca2+]i in freshly isolated and cultured NRVM for <1 day and ≥2 day for compatibility with the aortic myocytes. As expected, all of the cardiomyocytes from either group exhibited a robust increase in [Ca2+]i or the spontaneous Ca2+ transient frequency due to 10 μmol PE stimulation (Figure 4).
Intracellular Ca2+ signal response to α1-adrenergic activation in neonatal rat ventricular myocytes (NRVM). (A–C) Activating α1ARs with PE caused an increase in [Ca2+]i in freshly isolated NRVM (A) or in the frequency of spontaneous Ca2+ transients in primary NRVM cultured for 1 day (B) or 2 days (C). Numbers for each curve in all panels were from 7 to 15 separate experiments. The statistical data are given in the bottom panels of B and C. cP<0.01 vs control cardiomyocytes stimulated with vehicle.
Different α1AR subtypes in mediating Ca2+ signaling between vascular and cardiac myocytes
The different results between cultured VSMCs and cardiac myocytes after α1AR activation presumably suggest that distinctive receptor subtypes are responsible for the respective intracellular couplings. We thus investigated the functional α1AR subtype in the rat aorta and compared our data with previous results obtained in cardiomyocytes20, 24, 31, 32, 33. Similar to other studies9, 13, 14, 24, 32, we combined selective antagonists for each subtype with selective agonists to distinguish among contributions of the different subtypes to vasoconstriction. BMY 7378, a selective antagonist of α1D-ARs, attenuated the PE-induced constriction in a dose-dependent manner and completely abolished the constriction at a concentration of 30 μmol. Selective inhibition of α1A-ARs with 5-Mu (30 nmol) did not affect the PE effect, and A61603 (1 μmol), a highly selective α1A-AR agonist, did not induce any tension above baseline (data not shown). The irreversible antagonist chloroethylclonidine (CEC) at 10 μmol, the only available antagonist of α1B-ARs at present, inhibited the PE-induced contraction by approximately 30% (Figure 5), implying an involvement of α1B-ARs to some extent; however, these data do not provide a definite identification of the responsible subtype because of the low selectivity (5- to 10-fold) of CEC for α1B-AR over the other α1AR subtypes34.
α1D-Adrenergic receptor subtype plays a major role in phenylephrine-induced constriction in rat aorta. (A and B) Typical traces illustrate the effect of antagonists specific for individual α1AR subtypes on the PE-induced contraction in aortic rings as indicated in A and statistical results from 6 to 7 separate experiments for each antagonist (B). cP<0.01 vs DMSO+PE group. (C) A dose-response curve for selective α1D-AR antagonist BMY 7378 preventing 10 μmol PE-induced aortic contraction. The number at each point on the curve was from 5 to 7 separate experiments.
Taken together, these data demonstrated that α1AR functional relevance in the rat aorta and cardiac myocytes, especially for intracellular Ca2+ regulation, can be attributed to the activation of α1D-AR and α1A-AR subtypes, respectively, in agreement with previous reports13, 14, 15, 24, 31, 32, 33.
Differential distribution of α1D-ARs between freshly dispersed and cultured aortic myocytes
This study, thus far, has demonstrated that, unlike the functional receptor subtype in cardiomyocytes, α1D-ARs in VSMCs lost their sensitivity to activation after the cells were cultured. We then investigated the expression and subcellular distribution of α1D-ARs between freshly dissociated VSMCs (obvious Ca2+ signal response in more than 90% cells) and cultured VSMCs (no Ca2+ signal response at all) and compared these data with the distribution pattern of α1A-ARs in cultured cardiomyocytes.
An interesting report in α1D-AR transfected HEK293 cells has suggested that the treatment of culture medium with charcoal/dextran (C/D) increases the α1D-AR distribution on cell membranes and increases receptor's sensitivity to activation35. Thus, we determined the subcellular localization of α1AR subtypes with BODIPY-FL prazosin in live cells36 and using specific antibodies for individual subtypes in permeabilized cells. The tested cells were divided into four groups: freshly isolated VSMCs, VSMCs cultured for 2 days in DMEM in the presence of 2% charcoal/dextran (+C/D) or with the absence of 2% charcoal/dextran (-C/D), and NVRM cultured for 2 days.
As shown in Figures 6A and B, the binding signals for BODIPY-FL prazosin and anti-α1D-AR antibody were located both intracellularly and on the cell surface in freshly isolated VSMCs as well as in aorta tissue (data not shown), but membrane labeling disappeared in VSMC cultured −C/D, and was instead uniformly distributed inside the cytoplasm. Interestingly, cell membrane labeling could be detected in part of cultured VSMCs +C/D (membrane binding was detected in 34.67%±4.1%, n=84). Compared with α1D-ARs, α1A-AR binding appeared much less in VSMCs, but was apparent in most cultured NRVM, with a pattern of both cytosolic and cell membrane distributions.
Subcellular distributions of α1-adrenergic receptor subtypes and the effect of charcoal/dextran on α1D-adrenergic receptor localization, as well as intracellular Ca2+ response to phenylephrine in cultured rat myocytes. (A and B) Immunofluorescent images of freshly dispersed VSMCs. VSMCs cultured for >2 days in the absence or presence of charcoal/dextran (-C/D or +C/D), and NRVM cultured for 2 days stained with BODIPY FL prazosin (A) or antibodies specific for α1D-ARs or α1A-ARs (B) are shown in green. The nucleus was labeled with 8 μg/mL Hochest (blue). The arrows in panels A and B indicate relatively obvious cell membrane labeling of the antibody. The number for each staining was between 3 and 5 determinations, and the scale bar=10 μm for all images. (C) Typical traces for Ca2+ signal responses to PE in Fluo-4-loaded myocytes of each group. Numbers for each curve were from 4 to 7 separate experiments.
Accordingly, a robust internal Ca2+ signal response to 10 μmol PE was observed in both freshly isolated VSMCs and cultured NRVM. Further, while VSMCs cultured −C/D showed no response to PE (Figure 6C), an obvious PE-induced rise in [Ca2+]i (but lower than that in the freshly isolated VSMCs) could be induced in 29.5%±1.2% of tested VSMCs cultured +C/D (n=81), a response sensitive to the inhibitory effect of BMY 7378 (data not shown).
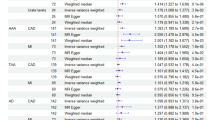
Finally, the protein expression of the α1AR subtypes in aorta tissue and cultured myocytes was analyzed by western-blotting. Compared with the labeling signal for α1A-ARs, α1D-ARs seemed to be the predominant receptor subtype in vascular muscle and were expressed at a higher level in the aorta tissue than in the cultured aortic myocytes, in accordance with the staining results. Additionally, the signal intensities for the α1D-AR bands were almost equal for VSMCs cultured −C/D and VSMCs cultured +C/D, indicating no significant effect of the C/D treatment on the native VSMC α1D-AR expression (Figure 7).
α1-Adrenergic receptor expression in aorta and cultured aortic smooth muscle cells. Representative immunoblotting of rat aortic tissue, NRVM, and 2-day cultured VSMCs in the absence or presence of C/D in DMEM labeled with antibodies for α1A-ARs or α1D-ARs from 3 separate experiments. The lysis sample quantity for the aorta is half that for cultured cell samples (see methods section).
Discussion
Our data showed that in rat or mouse aortas, a marked Ca2+-dependent contractile response was induced upon α1AR activation (Figures 1A and B, and 2A). In this response, the α1D-AR subtype played the most important role (Figure 5 and Refs 13, 14, 15). However, when VSMCs were isolated from the aorta and then cultured, the α1AR-associated Ca2+ signal response completely disappeared (Figures 1C and D, and 2B), a phenomenon also observed in other studies26, 37, 38. Under identical conditions, the cultured cardiac myocytes did exhibit a robust intracellular Ca2+ signal to α1AR activation (Figure 4) due to a different functional receptor subtype, the α1A-ARs, responsible for this effect (see Refs 24, and 31, 32, 33). Additionally, α1A-ARs in the cultured cardiac myocytes were found both intracellularly and at the cell membrane distributions, whereas α1D-ARs were most frequently concentrated intracellularly in cultured VSMCs (Figures 6A and B), consistent with existing research7, 8, 9, 10, 31. Interestingly, similar α1AR distribution patterns, α1 adrenergic-sensitive cell shortening and [Ca2+]i increases (as manifested in the cardiomyocytes) were clearly observable in most of the freshly isolated aortic myocytes, but disappeared completely in VSMCs cultured ≥ 2 days (Figures 3 and 6, and Table 1). Importantly, treating the culture medium with charcoal/dextran for 2 days caused the reappearance of α1D-ARs on the cell surface and the partial recovery of the α1AR-associated Ca2+ signal response in approximately 30% of the cultured VSMCs (Figure 6). Therefore, these results indicate a strong correlation between the cell membrane-expressed α1D-ARs and functional intracellular Ca2+ coupling, which is somehow lost during cell culture.
Charcoal/dextran treatment in the medium has been indicated to be capable of reducing steroid levels by absorbing free hormones, free fatty acids and various serum factors in fetal bovine serum39. Previous studies have shown that charcoal/dextran increases chloride channel expression in cultured epithelial cells40, increases α1D-AR expression on the cell membrane and also increases cells' responsiveness to receptor stimulation in α1D-AR recombinant HEK293 cells35. The current study further confirms the charcoal/dextran effect in native α1D-ARs in VSMCs. As there was no significant change in VSMC receptor-protein expression, except for the cellular localization owing to charcoal/dextran treatment, the mechanism responsible for α1D-AR insensitivity after cell culture may be partially due to some elements in the culture medium that either desensitizes the α1D-ARs by abrogating cell membrane insertion or facilitating internalization of the receptors in the native cells. Recently, several lines of evidence have implicated some critical factors for modulating α1D-AR functional expression at the cell membrane. For example, the truncation of 79 amino acids from the receptors' N-termini results in translocation of the α1D-ARs from intracellular compartments onto the plasma membrane, and a three- to four-fold increase in IP3 formation due to norepinephrine stimulation41. Additionally, dystrophin proteins, a type of intracellular anchor protein, have been identified as essential elements for α1D-AR but not for α1A- or α1B-AR functional expression for both in vitro and in vivo situations42. Therefore, all the previous studies describe a clear picture indicating the complexity of regulating α1D-AR expression at the cell membrane, a critical process for the receptor efficient functional performance.
In addition to the disappearance of cell membrane α1D-ARs, a marked reduction in receptor protein expression also occurred in the cultured VSMCs relative to the tissues studied (Figure 7). It is difficult to determine whether the reduction is secondary to the internalization of the receptors from the cell membrane or vice versa. Nevertheless, compared with the response in the freshly dispersed aortic myocytes, the significantly lower amplitude and duration of the PE-induced [Ca2+]i increase in the charcoal/dextran-treated cultured VSMCs (Figure 6C) suggest only a partial restoration of the native receptor activity by the treatment of culture medium with 2% charcoal/dextran.
In summary, the parallel investigations between vascular and cardiac myocytes indicate that first cell-surface expressed α1ARs are critical in triggering intracellular signal transduction cascades, especially for intracellular Ca2+ signaling. Second, α1D-ARs in the vessels primarily distribute intracellularly and on the cell membrane in situ, but are somehow reduced and abrogated from membrane localization after the VSMCs are cultured. Third, unlike the α1D-ARs of vascular myocytes, the α1ARs, actually likely α1A-ARs, in cardiac myocytes are not dramatically altered during the procedures of either cell isolation or culturing. These findings may help provide answers for the inconsistencies reported in α1D-AR function in vascular myocytes between in situ and in vitro studies. Treatment of the culture medium with charcoal/dextran can partially prevent native α1D-AR losses from the cell membrane and coupling intracellular signal machinery that occur in the cell culture process.
Author contribution
Prof Da-li LUO designed the research; Lin-lin FAN, Shuang REN, Hong ZHOU, Ying WANG, and Ping-xiang XU executed the research methods; Profs Jun-qi HE and Da-li LUO provided new reagents and analyzed data; and Lin-lin FAN and Shuang REN prepared the manuscript.
References
Wu D, Katz A, Lee CH, Simon MI . Activation of phospholipase C by alpha1-adrenergic receptors is mediated by the subunits of Gq family. J Biol Chem 1992; 267: 25798–802.
Graham RM, Perez DM, Hwa J, Piascik MT . Alpha1-adrenergic receptor subtypes. Molecular structure, function and signaling. Circ Res 1996; 78: 737–49.
Michelotti GA, Price DT, Schwinn DA . Alpha1-adrenergic receptor regulation: basic science and clinical implications. Pharmacol Ther 2000; 88: 281–309.
Albert AP, Large WA . Signal transduction pathways and gating mechanisms of native TRP-like cation channels in vascular myocytes. J Physiol 2006; 570 (Pt 1): 45–51.
Zhong H, Minneman KP . Alpha1-adrenoceptor subtypes. Eur J Pharmacol 1999; 375: 261–76.
Piascik MT, Perez DM . Alpha1-adrenergic receptors: new insights and directions. J Pharmacol Exp Ther 2001; 298: 403–10.
Milligan G . Exploring the dynamics of regulation of G protein-coupled receptors using green fluorescent protein. Br J Pharmacol 1999; 128: 501–10.
Chalothorn D, McCune DF, Edelmann SE, Garcia-Cazarin ML, Tsujimoto G, Piascik MT . Differences in the cellular localization and agonist-mediated internalization properties of the alpha1-adrenoceptor subtypes. Mol Pharmacol 2002; 61: 1008–16.
Theroux TL, Esbenshade TA, Peavy RD . Minneman KP . Coupling efficiencies of human alpha1-adrenergic receptor subtypes: titration of receptor density and responsiveness with inducible and repressible expression vectors. J Pharmacol Exp Ther 1996; 50: 1376–87.
Uberti MA, Hall RA, Minneman KP . Subtype specific dimerization of alpha1-adrenoceptors: effects on receptor expression and pharmacological properties. Mol Pharmacol 2003; 64: 1379–90.
Hein P, Michel MC . Signal transduction and regulation: Are all alpha1-adrenergic receptor subtypes created equal? Biochem Pharmacol 2007; 73: 1097–106.
Perez DM . Structure–function of alpha1-adrenergic receptors. Biochem Pharmacol 2007; 73: 1051–62.
Kenny BA, Chalmers DH, Philpott PC, Naylor AM . Characterization of an alpha1D-adrenoceptor mediating the contractile response of rat aorta to noradrenaline. Br J Pharmacol 1995; 115: 981–6.
Gisbert R, Pérez-Vizcaino F, Cogolludo AL, Noguera MA, Ivorra MD, Tamargo J, et al. Cytosolic Ca2+ and phosphoinositide hydrolysis linked to constitutively active alpha1D-adrenoceptors in vascular smooth muscle. J Pharmacol Exp Therap 2003; 305: 1006–14.
Tanoue A, Nasa Y, Koshimizu T, Shinoura H, Oshikawa S, Kawai T, et al. The alpha1D-adrenergic receptor directly regulates arterial blood pressure via vasoconstriction. J Clin Invest 2002; 109: 765–75.
Hosoda C, Koshimizu T, Tanoue A, Nasa Y, Oikawa R, Tomabechi T, et al. Two alpha1-adrenergic receptor subtypes regulating the vasopressor response have differential roles in blood pressure regulation. Mol Pharmacol 2005; 67: 912–22.
Rudner XL, Berkowitz DE, Booth JV, Funk BL, Cozart KL, D'Amico EB, et al. Subtype specific regulation of human vascular alpha1-adrenergic receptors by vessel bed and age. Circ 1999; 100: 2336–43.
Tanoue A, Koba M, Miyawaki S, Koshimizu T, Hosoda C, Oshikawa S, et al. Role of the alpha1D-adrenegric receptor in the development of salt-induced hypertension. Hypertension 2002; 40: 101–6.
Oliver E, Martí D, Montó F, Flacco N, Moreno L, Barettino DM, et al. The impact of alpha1-adrenoceptors up-regulation accompanied by the impairment of β-adrenergic vasodilatation in hypertension. J Pharmacol Exp Ther 2009; 328: 982–90.
Chaulet H, Lin F, Guo J, Owens WA, Michalicek J, Kesteven SH, et al. Sustained augmentation of cardiac alpha1A-adrenergic drive results in pathological remodeling with contractile dysfunction, progressive fibrosis and reactivation of matricellular protein genes. J Mol Cell Cardiol 2006; 40: 540–52.
Luo D, Yang D, Lan X, Li K, Li X, Chen J, et al. Nuclear Ca2+ sparks and waves mediated by inositol 1,4,5-trisphoshate receptors in neonatal rat cardiomyocytes. Cell Calcium 2008; 43: 165–74.
Hunton DL, Lucchesi PA, Pang Y, Cheng X, Dell'Italia LJ, Marchase RB . Capacitative calcium entry contributes to nuclear factor of activated T-cells nuclear translocation and hypertrophy in cardiomyocytes. J Biol Chem 2002; 277: 14266–73.
García KD, Shah T, García J . Immunolocalization of type 2 inositol 1,4,5-trisphosphate receptors in cardiac myocytes from newborn mice. Am J Physiol Cell Physiol 2004; 287: C1048–C57.
Autelitano DJ, Woodcock EA . Selective activation of alpha1A-adrenergic receptors in neonatal cardiac myocytes is sufficient to cause hypertrophy and differential regulation of alpha1-adrenergic receptor subtype mRNAs. J Mol Cell Cardiol 1998; 30: 1515–23.
Luo D, Nakazawa M, Ishibashi T, Kato K, Imai S . Putative, selective inhibitors of sarcoplasmic reticulum Ca2+-pump ATPase inhibit relaxation by nitroglycerin and atrial natriuretic factor of the rabbit aorta contracted by phenylephrine. J Pharmacol Exp Ther 1993; 265: 1187–92.
Zhou H, Iwasaki H, Nakamura T, Nakamura K, Maruyama T, Hamano S, et al. 2-Aminoethyl diphenylborinate analogues: Selective inhibition for store-operated Ca2+ entry. Biochem Biophys Res Commun 2007; 352: 277–82.
Rapps JA, Sturek M, Jones AW, Parker JL . Altered reactivity of coronary arteries located distal to a chronic coronary occlusion. Am J Physiol 1997; 273 (4 Pt 2): H1879–H87.
Villalba N, Stankevicius E, Garcia-Sacristán A, Simonsen U, Prieto D . Contribution of both Ca2+ entry and Ca2+ sensitization to the alpha1-adrenergic vasoconstriction of rat penile small arteries. Am J Physiol Heart Circ Physiol 2007; 292: H1157–H69.
Erlinge D . Extracellular ATP: a central player in the regulation of vascular smooth muscle phenotype. Focus on “Dual role of PKA in phenotype modulation of vascular smooth muscle cells by extracellular ATP”. Am J Physiol Cell Physiol 2004, 287: C260–2.
Serir K, Hayoz S, Fanchaouy M, Beny JL, Bychkov R . A delayed ATP-elicited K+ current in freshly isolated smooth muscle cells from mouse aorta. Br J Pharmacol 2006; 147: 45–54.
Woodcock EA, Du XJ, Reichelt ME, Graham RM . Cardiac alpha1-adrenergic drive in pathological remodeling. Cardiovasc Res 2008; 77: 452–62.
Knowlton KU, Michel MC, Itani M, Shubeita HE, Ishihara K, Brown JH . The alpha1A-adrenergic receptor subtype mediates biochemical, molecular, and morphologic features of cultured myocardial cell hypertrophy. J Biol Chem 1993; 268: 15374–80.
Luo D, Gao J, Fan L, Tang Y, Zhang Y, Han Q . Receptor subtype involved in alpha1-adrenergic receptor-mediated Ca2+ signaling in cardiomyocytes. Acta Pharmacol Sin 2007; 28: 921–1086.
Hanft G, Gross G . Subclassification of alpha1-adrenoceptor recognition sites by urapidil derivatives and other selective antagonists. Br J Pharmacol 1989; 97: 691–700.
Khattar SK, Bora RS, Priyadarsiny P, Gautam A, Gupta D, Tiwari A, et al. Molecular cloning, stable expression and cellular localization of human alpha1-adrenergic receptor subtypes: effect of charcoal/dextran treated serum on expression and localization of alpha1D-adrenergic receptor. Biotechnol Lett 2006; 28: 1731–9.
Mackenzie JF, Daly CJ, Pedian JI, Mcgrath JC . Quantitative imaging in live human cells reveals Intracellular alpha1-adrenoceptor ligand-binding sites. J Pharmacol Exp Ther 2000; 294: 434–43.
Woodsome TP, Polzin A, Kitazawa K, Eto M . Kitazawa T . Agonist- and depolarization-induced signals for myosin light chain phosphorylation and force generation of cultured vascular smooth muscle cells. J Cell Sci 2006; 119: 1769–80.
Koshimizu T, Tsujimoto G, Hirasawa A, Kitagawa Y, Tanoue A . Carvedilol selectively inhibits oscillatory intracellular calcium changes evoked by human alpha1D- and alpha1B-adrenergic receptors. Cardiovas Res 2004; 63: 662–72.
Lindquist DL, de Alarcon PA . Charcoal-dextran treatment of fetal bovine serum removes an inhibitor of human CFU-megakaryocytes. Exp Hematol 1987; 15: 234–38.
Tsang LL, Chan LN, Liu CQ, Chan HC . Effect of phenol red and steroid hormones on cystic fibrosis transmembrane conductance regulator in mouse endometrial epithelial cells. Cell Biol Int 2001; 25: 1021–4.
Hague C, Chen Z, Pupo AS, Schulte NA, Toews ML, Minneman KP . The N terminus of the human alpha1D-adrenergic receptor prevents cell surface expression. J Pharmacol Exp Ther 2004; 309: 388–97.
Lyssand JS, DeFino MC, Tang X, Hertz AL, Feller DB, Wacker JL, et al. Blood pressure is regulated by an alpha1D-adrenergic receptor/dystrophin signalosome. J Biol Chem 2008; 283: 18792–800.
Acknowledgements
This study was supported by grants from the National Natural Science Foundation (No 30772574), the Beijing Municipal Project for Developing Advanced Human Resources for Higher Education, the Scientific Research Common Program of the Beijing Municipal Commission of Education (DL), and the Beijing Natural Science Foundation (No 7082018).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fan, Ll., Ren, S., Zhou, H. et al. α1D-Adrenergic receptor insensitivity is associated with alterations in its expression and distribution in cultured vascular myocytes. Acta Pharmacol Sin 30, 1585–1593 (2009). https://doi.org/10.1038/aps.2009.160
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.160