Abstract
The anti-tumour effect of radiotherapy beyond the treatment field—the abscopal effect—has garnered much interest1. However, the potentially deleterious effect of radiation in promoting metastasis is less well studied. Here we show that radiotherapy induces the expression of the EGFR ligand amphiregulin in tumour cells, which reprogrammes EGFR-expressing myeloid cells toward an immunosuppressive phenotype and reduces phagocytosis. This stimulates distant metastasis growth in human patients and in pre-clinical mouse tumour models. The inhibition of these tumour-promoting factors induced by radiotherapy may represent a novel therapeutic strategy to improve patient outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
199,00 € per year
only 3,90 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The scRNA-seq data have been deposited at the Gene Expression Omnibus (GEO) under accession GSE250375. The bulk RNA-sequencing data have been deposited at the GEO under accession GSE291151. The microarray data of the patients with advanced solid tumours enrolled in the clinical trial (ClinicalTrials.gov ID: NCT026083851) are available from the corresponding author upon reasonable request. The human LUSC genomic and clinical data were derived from the TCGA Research Network (http://cancergenome.nih.gov) using the Xena platform (https://xena.ucsc.edu/). Publicly available datasets used: mouse reference genome (mm10-2020A): https://www.ncbi.nlm.nih.gov/grc/mouse, Reactome: https://reactome.org/ and Molecular Signature Database: https://www.gsea-msigdb.org/gsea/msigdb/index.jsp. All data supporting the findings of this study are available within the Article and its Supplementary Information. Source data are provided with this paper.
Code availability
The code used for the custom tissue specific AI-based cell segmentation model is available on Github (https://github.com/apiffko/IF.mono.quantif) and has been archived on Zenodo (https://doi.org/10.5281/zenodo.14982759 (ref. 78)).
References
Weichselbaum, R. R., Liang, H., Deng, L. & Fu, Y. X. Radiotherapy and immunotherapy: a beneficial liaison? Nat. Rev. Clin. Oncol. 14, 365–379 (2017).
Orth, M. et al. Current concepts in clinical radiation oncology. Radiat. Environ. Biophys. 53, 1–29 (2014).
Lomax, M. E., Folkes, L. K. & O’Neill, P. Biological consequences of radiation-induced DNA damage: relevance to radiotherapy. Clin. Oncol. 25, 578–585 (2013).
Lynch, C., Pitroda, S. P. & Weichselbaum, R. R. Radiotherapy, immunity, and immune checkpoint inhibitors. Lancet Oncol. 25, e352–e362 (2024).
Liang, H. et al. Host STING-dependent MDSC mobilization drives extrinsic radiation resistance. Nat. Commun. 8, 1736 (2017).
Jiménez-Cortegana, C., Galassi, C., Klapp, V., Gabrilovich, D. I. & Galluzzi, L. Myeloid-derived suppressor cells and radiotherapy. Cancer Immunol. Res. 10, 545–557 (2022).
Pitroda, S. P., Chmura, S. J. & Weichselbaum, R. R. Integration of radiotherapy and immunotherapy for treatment of oligometastases. Lancet Oncol. 20, e434–e442 (2019).
Pointer, K. B., Pitroda, S. P. & Weichselbaum, R. R. Radiotherapy and immunotherapy: open questions and future strategies. Trends Cancer 8, 9–20 (2022).
Wang, L. et al. RNA m6A methylation and MDSCs: roles and therapeutic implications for radiotherapy. Med 4, 863–874 (2023).
Shoyab, M., Plowman, G., McDonald, V., Bradley, J. G. & Todaro, G. J. Structure and function of human amphiregulin: a member of the epidermal growth factor family. Science 243, 1074–1076 (1989).
Shoyab, M., McDonald, V. L., Bradley, J. G. & Todaro, G. J. Amphiregulin: a bifunctional growth-modulating glycoprotein produced by the phorbol 12-myristate 13-acetate-treated human breast adenocarcinoma cell line MCF-7. Proc. Natl. Acad. Sci. USA 85, 6528–6532 (1988).
Zaiss, D. M. W. et al. Amphiregulin enhances regulatory T cell-suppressive function via the epidermal growth factor receptor. Immunity 38, 275–284 (2013).
Zaiss, D. M. W., Gause, W. C., Osborne, L. C. & Artis, D. Emerging functions of amphiregulin in orchestrating immunity, inflammation, and tissue repair. Immunity 42, 216–226 (2015).
Minutti, C. M. et al. Epidermal growth factor receptor expression licenses type-2 helper T cells to function in a T cell receptor-independent fashion. Immunity 47, 710–722.e6 (2017).
Busser, B., Sancey, L., Brambilla, E., Coll, J. L. & Hurbin, A. The multiple roles of amphiregulin in human cancer. Biochim. Biophys. Acta 1816, 119–131 (2011).
Berasain, C. & Avila, M. A. Amphiregulin. Semin. Cell Dev. Biol. 28, 31–41 (2014).
Shao, J. & Sheng, H. Amphiregulin promotes intestinal epithelial regeneration: roles of intestinal subepithelial myofibroblasts. Endocrinology 151, 3728–3737 (2010).
Luke, J. J. et al. Safety and clinical activity of pembrolizumab and multisite stereotactic body radiotherapy in patients with advanced solid tumors. J. Clin. Oncol. 36, 1611–1618 (2018).
Mulder, K. et al. Cross-tissue single-cell landscape of human monocytes and macrophages in health and disease. Immunity 54, 1883–1900.e5 (2021).
Georgiades, P. et al. vavCre transgenic mice: a tool for mutagenesis in hematopoietic and endothelial lineages. Genesis 34, 251–256 (2002).
Johnstone, C. N. et al. Functional and molecular characterisation of EO771.LMB tumours, a new C57BL/6-mouse-derived model of spontaneously metastatic mammary cancer. Dis. Model. Mech. 8, 237–251 (2015).
McElrath, C. et al. Critical role of interferons in gastrointestinal injury repair. Nat. Commun. 12, 2624 (2021).
Gilmore, J. L. et al. Amphiregulin-EGFR signaling regulates PTHrP gene expression in breast cancer cells. Breast Cancer Res. Treat. 110, 493–505 (2008).
Miyawaki, M. et al. Enhanced phosphorylation of the epidermal growth factor receptor at the site of tyrosine 992 in esophageal carcinomas. APMIS 116, 1097–1106 (2008).
Bestvina, C. M. et al. A phase 1 trial of concurrent or sequential ipilimumab, nivolumab, and stereotactic body radiotherapy in patients with stage IV NSCLC study. J. Thorac. Oncol. 17, 130–140 (2022).
Van Der Maaten, L. & Hinton, G. Visualizing Data using t-SNE. J. Mach. Learn. Res. 9, 2579–2605 (2008).
Swirski, F. K., Hilgendorf, I. & Robbins, C. S. From proliferation to proliferation: monocyte lineage comes full circle. Semin. Immunopathol. 36, 137–148 (2014).
Noy, R. & Pollard, J. W. Tumor-associated macrophages: from mechanisms to therapy. Immunity 41, 49–61 (2014).
Wang, T. et al. Influenza-trained mucosal-resident alveolar macrophages confer long-term antitumor immunity in the lungs. Nat. Immunol. 24, 423–438 (2023).
Wang, L. et al. YTHDF2 inhibition potentiates radiotherapy antitumor efficacy. Cancer Cell 41, 1294–1308 (2023).
Miller, B. C. et al. Subsets of exhausted CD8+ T cells differentially mediate tumor control and respond to checkpoint blockade. Nat. Immunol. 20, 326–336 (2019).
Mack, M. et al. Expression and characterization of the chemokine receptors CCR2 and CCR5 in mice. J. Immunol. 166, 4697–4704 (2001).
Lecoultre, M., Dutoit, V. & Walker, P. R. Phagocytic function of tumor-associated macrophages as a key determinant of tumor progression control: a review. J. Immunother. Cancer 8, e001408 (2020).
Platen, C., Dreschers, S., Reiss, L. K., Wappler, J. & Orlikowsky, T. W. Amphiregulin regulates phagocytosis-induced cell death in monocytes via EGFR and matrix metalloproteinases. Mediators Inflamm. 2018, 4310419 (2018).
Hsu, Y.-L. et al. Lung tumor-associated dendritic cell-derived amphiregulin increased cancer progression. J. Immunol. 187, 1733–1744 (2011).
Ebott, J. et al. Enhanced amphiregulin exposure promotes modulation of the high grade serous ovarian cancer tumor immune microenvironment. Front. Pharmacol. 15, 1375421 (2024).
Lu, J. et al. Reprogramming of TAMs via the STAT3/CD47-SIRPα axis promotes acquired resistance to EGFR-TKIs in lung cancer. Cancer Lett. 564, 216205 (2023).
Schust, J., Sperl, B., Hollis, A., Mayer, T. U. & Berg, T. Stattic: a small-molecule inhibitor of STAT3 activation and dimerization. Chem. Biol. 13, 1235–1242 (2006).
Jaiswal, S. et al. CD47 is upregulated on circulating hematopoietic stem cells and leukemia cells to avoid phagocytosis. Cell 138, 271–285 (2009).
Oldenborg, P. A., Gresham, H. D. & Lindberg, F. P. CD47-signal regulatory protein α (Sirpα) regulates Fcγ and complement receptor-mediated phagocytosis. J. Exp. Med. 193, 855–862 (2001).
Tsai, R. K. & Discher, D. E. Inhibition of ‘self’ engulfment through deactivation of myosin-II at the phagocytic synapse between human cells. J. Cell Biol. 180, 989–1003 (2008).
Ready, N. et al. Chemoradiotherapy and gefitinib in stage III non-small cell lung cancer with epidermal growth factor receptor and KRAS mutation analysis: Cancer and Leukemia Group B (CALEB) 30106, a CALGB-stratified phase II trial. J. Thorac. Oncol. 5, 1382–1390 (2010).
Kelly, K. et al. Phase III trial of maintenance gefitinib or placebo after concurrent chemoradiotherapy and docetaxel consolidation in inoperable stage III non-small-cell lung cancer: SWOG S0023. J. Clin. Oncol. 26, 2450–2456 (2008).
Wrona, A., Dziadziuszko, R. & Jassem, J. Combining radiotherapy with targeted therapies in non-small cell lung cancer: Focus on anti-EGFR, anti-ALK and anti-angiogenic agents. Transl. Lung Cancer Res. 10, 2032–2047 (2021).
Ishikawa, N. et al. Increases of amphiregulin and transforming growth factor-α in serum as predictors of poor response to gefitinib among patients with advanced non-small cell lung cancers. Cancer Res. 65, 9176–9184 (2005).
Kaplan, H. S. & Murphy, E. D. The effect of local roentgen irradiation on the biological behavior of a transplantable mouse carcinoma. i. Increased frequency of pulmonary metastasis. J. Natl Cancer Inst. 9, 407–413 (1949).
Sundahl, N., Duprez, F., Ost, P., De Neve, W. & Mareel, M. Effects of radiation on the metastatic process. Mol. Med. 24, 16 (2018).
Nishiga, Y. et al. Radiotherapy in combination with CD47 blockade elicits a macrophage-mediated abscopal effect. Nat. Cancer 3, 1351–1366 (2022).
Lanaya, H. et al. EGFR has a tumour-promoting role in liver macrophages during hepatocellular carcinoma formation. Nat. Cell Biol. 16, 972–981 (2014).
Wang, X. et al. EGFR is a master switch between immunosuppressive and immunoactive tumor microenvironment in inflammatory breast cancer. Sci. Adv. 8, eabn7983 (2022).
Nickerson, N. K., Mill, C. P., Wu, H. J., Riese, D. J. & Foley, J. Autocrine-derived epidermal growth factor receptor ligands contribute to recruitment of tumor-associated macrophage and growth of basal breast cancer cells in vivo. Oncol. Res. 20, 303 (2013).
Chayangsu, C., Khunsri, S., Sriuranpong, V. & Tanasanvimon, S. The correlations between serum amphiregulin and other clinicopathological factors in colorectal cancer. J. Gastrointest. Oncol. 8, 980–984 (2017).
Kim, S. A. et al. Amphiregulin can predict treatment resistance to palliative first-line cetuximab plus FOLFIRI chemotherapy in patients with RAS wild-type metastatic colorectal cancer. Sci. Rep. 11, 23803 (2021).
Xu, Q. et al. Targeting amphiregulin (AREG) derived from senescent stromal cells diminishes cancer resistance and averts programmed cell death 1 ligand (PD-L1)-mediated immunosuppression. Aging Cell 18, e13027 (2019).
Luke, J. J. et al. Improved survival associated with local tumor response following multisite radiotherapy and pembrolizumab: secondary analysis of a phase I trial. Clin. Cancer Res. 26, 6437–6444 (2020).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
Arpaia, N. et al. A distinct function of regulatory T cells in tissue protection. Cell 162, 1078–1089 (2015).
Lee, T.-C. & Threadgill, D. W. Generation and validation of mice carrying a conditional allele of the epidermal growth factor receptor. Genesis 47, 85–92 (2009).
Doki, Y. et al. Mediastinal lymph node metastasis model by orthotopic intrapulmonary implantation of Lewis lung carcinoma cells in mice. Br. J. Cancer 79, 1121–1126 (1999).
Wang, L. M. et al. Validation of an orthotopic non-small cell lung cancer mouse model, with left or right tumor growths, to use in conformal radiotherapy studies. PLoS ONE 18, e0284282 (2023).
Stringer, C., Wang, T., Michaelos, M. & Pachitariu, M. Cellpose: a generalist algorithm for cellular segmentation. Nat. Methods 18, 100–106 (2021).
Pachitariu, M. & Stringer, C. Cellpose 2.0: how to train your own model. Nat. Methods 19, 1634–1641 (2022).
Youden, W. J. Index for rating diagnostic tests. Cancer 3, 32–35 (1950).
Otsu, N. A threshold selection method from gray-level histograms. IEEE Trans. Syst. Man Cybern. 9, 62–66 (1979).
Levine, J. H. et al. Data-driven phenotypic dissection of aml reveals progenitor-like cells that correlate with prognosis. Cell 162, 184–197 (2015).
Van Gassen, S. et al. FlowSOM: using self-organizing maps for visualization and interpretation of cytometry data. Cytometry A 87, 636–645 (2015).
Li, B. et al. Cumulus provides cloud-based data analysis for large-scale single-cell and single-nucleus RNA-seq. Nat. Methods 17, 793–798 (2020).
Wolf, F. A., Angerer, P. & Theis, F. J. SCANPY: large-scale single-cell gene expression data analysis. Genome Biol. 19, 15 (2018).
Satija, R., Farrell, J. A., Gennert, D., Schier, A. F. & Regev, A. Spatial reconstruction of single-cell gene expression data. Nat. Biotechnol. 33, 495–502 (2015).
Korsunsky, I. et al. Fast, sensitive and accurate integration of single-cell data with Harmony. Nat. Methods 16, 1289–1296 (2019).
Traag, V. A., Waltman, L. & van Eck, N. J. From Louvain to Leiden: guaranteeing well-connected communities. Sci. Rep. 9, 5233 (2019).
Street, K. et al. Slingshot: cell lineage and pseudotime inference for single-cell transcriptomics. BMC Genomics 19, 477 (2018).
La Manno, G. et al. RNA velocity of single cells. Nature 560, 494–498 (2018).
Bergen, V., Lange, M., Peidli, S., Wolf, F. A. & Theis, F. J. Generalizing RNA velocity to transient cell states through dynamical modeling. Nat. Biotechnol. 38, 1408–1414 (2020).
Gillespie, M. et al. The reactome pathway knowledgebase 2022. Nucleic Acids Res. 50, D687–D692 (2022).
Yang, Y. & Li, B. A streamlined method for signature score calculation. GitHub https://github.com/lilab-bcb/pegasus/blob/master/signature_score.pdf (2025).
Goldman, M. J. et al. Visualizing and interpreting cancer genomics data via the Xena platform. Nat. Biotechnol. 38, 675–678 (2020).
ldonle & apiffko. apiffko/IF.mono.quantif: IF.mono.quantif (v.1.0.0). Zenodo https://doi.org/10.5281/zenodo.14982760 (2025).
Acknowledgements
The authors thank A. Arina, C. Maire, M. F. Allega and A. J. Bilecz for scientific discussions and input; J. Wang, X. Huang and R. Torres for technical assistance; and A. K. Huser for editing the manuscript. Research reported in this publication was supported in part by grants from the Ludwig Foundation, the Chicago Tumor Institute, by the National Cancer Institute (NCI) of the National Institutes of Health (NIH) under Award Numbers U54CA274291 and R01CA262508 to R.R.W., as well as by generous gifts from Mr. and Mrs. V. Foglia and the Foglia foundation, Mr. and Mrs. D. Kozin and Mr. and Mrs. J. Weichselbaum. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. A. Piffkó and J.H. are recipients of a Walter Benjamin scholarship provided by the German Research Foundation (Deutsche Forschungsgemeinschaft (DFG); A. Piffkó, 455353745; J.H., 459327389). A. Panda was supported by a T32GM007281/GM/NIGMS grant. J.B. was supported by a Clinical Therapeutics Training Grant (T32GM007019) and a NIH/NCI grant (K12CA139160). E.L. is supported by a NIH/NCI R35 CD264619. R.S.R. was supported by NIH/NIGMS R01 GM149073. We acknowledge technical support from the University of Chicago Human Tissue Resource Center (RRID:SCR_019199), Animal Studies Core (P30CA014599), Microscopy Core (P30CA014599), Cellular Screening Core (RRID:SCR_017914), Functional Genomics Core (P30CA014599, RRID:SCR_019196), and Flow Cytometry Core (P30CA014599, RRID: SCR_017760). Grant numbers: Ludwig Center for Metastasis Research, Chicago Tumor Institute, Ludwig Foundation, NIH/NCI U54CA274291 and NIH/NCI R01CA262508 (R.R.W.); Walter Benjamin scholarships: German Research Foundation (Deutsche Forschungsgemeinschaft (DFG)) 455353745 (A. Piffkó) and 459327389 (J.H.); NIH/NCI R35 CA264619 (E.L.), T32GM007281 (A. Panda); NIH Clinical Therapeutics Training Grant T32GM007019 and NIH/NCI grant K12CA139160 (J.B.); and NIH/NIGMS R01 GM149073 (R.S.R.). Technical support was provided through resource core funding: University of Chicago Human Tissue Resource Center SCR_019199; Animal Studies Core SCR_021806; Microscopy Core SCR_019197; Cellular Screening Core SCR_017914; Functional Genomics Core SCR_019196 and Flow Cytometry Core SCR_017760.
Author information
Authors and Affiliations
Contributions
A. Piffkó, K.Y., Y.F., H.L.L. and R.R.W. conceived the study. A. Piffkó, K.Y. and H.L.L. designed the experiments. A. Piffkó, K.Y., K.T., J.H., E.Z.N., C.W., D.C., Y.F., J.B. and L.W. performed the experiments. A. Piffkó, K.Y. and L.W. prepared samples for scRNA-seq, which A. Panda analysed with support from A. Piffkó and K.Y. J.B., L.D. and K.Z. performed additional data analysis. K.T. performed confocal microscopy under supervision from R.S.R., A. Piffkó, K.Y., J.H., K.T. and S.P.P. analysed experimental data. H.L.L., E.L., D.G.T., S.J.C., E.E.V., R.S.R., M.M., C.H. and R.R.W. contributed resources. A. Piffkó, K.Y., S.P.P., H.L.L. and R.R.W. drafted and finalized the manuscript with input from all other authors.
Corresponding author
Ethics declarations
Competing interests
R.R.W. has stock and other ownership interests with Boost Therapeutics, Immvira, Reflexion Pharmaceuticals, Coordination Pharmaceuticals, Magi Therapeutics and Oncosenescence. He has served in a consulting or advisory role for Aettis, Astrazeneca, Coordination Pharmaceuticals, Genus, Merck Serono S.A., Nano proteagen, NKMax America and Shuttle Pharmaceuticals. He has a patent pending entitled ‘Methods and Kits for Diagnosis and Triage of Patients with Colorectal Liver Metastases’ (PCT/US2019/028071). He has received research grant funding from Varian and Regeneron. He has received compensation including travel, accommodations, or expense reimbursement from Astrazeneca, Boehringer Ingelheim and Merck Serono S.A. C.H. has stock and other ownership interests with Accent Therapeutics and Aferna Green. C.H. is a scientific advisory board member of Aferna Green and Rona Therapeutics. A. Piffkó has consulted for Related Sciences/Danger Bio and owns equity in Danger Bio. E.L. receives research funding to study the biology of ovarian cancer from AbbVie through The University of Chicago that is unrelated to this work. A patent application has been submitted by A. Piffkó, H.L.L., S.P.P. and R.R.W and is pending at the date of publication. The other authors declare no competing interests.
Peer review
Peer review information
Nature thanks Leila Akkari and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
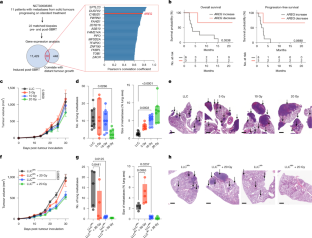
Extended Data Fig. 1 Characterization of LLC lung metastasis model reveals dose-dependent AREG secretion from tumour tissue following RT.
a, Top 20 RT-induced pathways correlated with distant metastasis progression in patients (Ingenuity Pathway Analysis); pathways including AREG are highlighted in red. b, Kaplan-Meier survival curves of The Cancer Genome Atlas (TCGA) lung squamous cell carcinoma (LUSC) patients undergoing RT, stratified by tumour AREG expression. Log-rank (Mantel-Cox) test. c, Experimental setup: RT applied to either LLC flank tumours (1), or a non-tumour bearing (NTB) hindlimb (2). Serum, lung, skin, tumour and muscle tissues were collected five days post-RT for AREG quantification by ELISA. Created in BioRender (Piffkó, A. (2025) https://BioRender.com/t23f494). d, AREG concentration in tumour (left), serum (centre), and lung (right) of LLC tumour-bearing mice five days post-RT, measured by ELISA, n = 5 mice per group. One-way ANOVA, Šídák’s test. e, AREG concentration in serum (left), muscle (centre), and skin (right) of non-tumour-bearing mice five days after RT of the hindlimb, measured by ELISA, n = 3 mice per group. One-way ANOVA, Šídák’s test. f, Growth curve of LLC flank tumours ± 20 Gy in Vav1ΔAreg and Aregflx/flx mice, n = 4 mice in Aregflx/flx, n = 5 in all others. g, Number (left) of macroscopic metastases and weight of lungs (right) in Vav1ΔAreg and Aregflx/flx mice, n = 4 mice per group. One-way ANOVA, Šídák’s test. h, Number of lung metastases (left), and mean size of the five largest metastases per lung area (right) on days 12, 15, and 18 following subcutaneous LLC tumour injection, n = 4 mice per group. i, H&E staining. Black arrows indicate metastatic lesions. j, Number of lung metastases (left), and mean size of the five largest metastases per lung area (right) of day 8 RT group, n = 7 mice per group. Two-sided Mann-Whitney test. k, Number of lung metastases (left), and mean size of the five largest metastases per lung area (right) of day 20 RT group, n = 8 mice in LLC group, n = 6 in 20 Gy group. Unpaired two-sided t-test. l, H&E staining. Black arrows indicate metastatic lesions. m, Serum AREG-concentration post-RT, measured by ELISA at indicated timepoints, (from left to right; n = 5, n = 6, n = 7, n = 7 mice per group). One-way ANOVA, Šídák’s test. n, Linear regression of serum AREG concentration (pg/mL) five days post-RT vs. flank tumour size at RT. blue = d8 RT, red = d20 RT. Pearson’s R and P values shown. Data are shown as mean ± SEM; box plots show median (Q2), Q1–Q3, and whiskers (min–max).
Extended Data Fig. 2 Characterization of spontaneously metastatic orthotopic lung LLC and subcutaneous EO771 – LMB models.
a, Areg upregulation in LLCAR+ and LLCAR− cells after 4 Gy RT in vitro, measured by RT-qPCR 3 h post-RT. One-way ANOVA, Šídák’s test. n = 3 technical repeats. b, AREG concentration in flank tumour lysate ± 20 Gy RT, measured by ELISA 5 days post-RT, n = 5 mice in AR+ groups, n = 4 in AR- groups. One-way ANOVA, Šídák’s test. c, Serum AREG concentration in tumour-bearing mice ± 20 Gy RT, measured by ELISA. Blood draw timepoints post-RT as indicated, ctrl - n = 3 non-tumour bearing mice, n = 5 mice in other groups. Two-way ANOVA, Tukey’s test. d, CT-images of orthotopic LLCAR+ and LLCAR− tumours on days 8, 11, and 14 post-injection. White asterisks/red highlights indicate tumours. e, Growth curves of LLCAR+ and LLCAR− orthotopic lung tumours ± 8 or 12 Gy CT-guided RT. n = 6 mice per group. Two-way ANOVA, Šídák’s test. f, Serum AREG concentration of LLCAR+ and LLCAR− orthotopic lung tumour-bearing mice five days after 8 or 12 Gy RT, measured by ELISA, n = 4 mice in all groups. One-way ANOVA, Šídák’s test. g, Number of contralateral lung metastases (left) and mean size of the five largest metastases per contralateral lung area (right) from LLCAR+ and LLCAR− orthotopic tumours (n = 4 in LLCAR+, n = 5 in LLCAR−, n = 6 mice in others). One-way ANOVA, Šídák’s test. h, H&E staining of LLCAR+ and LLCAR− orthotopic lung tumours. Black arrows indicate contralateral intrapulmonary metastatic lesions, white asterisks = orthotopic tumours, LN = extrapulmonary, intrathoracic lymph node metastasis. i, AREG MFI in LMB and LLC tumour cells post 4 Gy and 8 Gy RT in vitro, determined by flow cytometry. n = 2 technical repeats in LLC + 8 Gy, n = 3 in all other groups. j, Growth curves of LMB flank tumours ± RT with indicated doses, n = 4 mice in all groups, two independent experiments. Two-way ANOVA, Tukey’s test. k, Number of LMB lung metastases (left) and mean size of the five largest lung metastases per lung area (right), n = 5 mice in LMB and 5 Gy groups, n = 4 in 10 Gy and 20 Gy groups. One-way ANOVA, Dunnett’s test. l, H&E staining. Black arrows indicate metastatic lesions. RT doses as indicated. m, Areg upregulation in LMBAR+ and LMBAR− cells after 4 Gy RT in vitro post-RT, RT-qPCR. One-way ANOVA, Šídák’s test. n = 3 technical repeats. n, Growth curves of LMBAR+ and LMBAR− flank tumours ± 5 Gy; n = 4 mice in LMBAR− + 5 Gy group, n = 5 mice in all others. o, Number of lung metastases (left), and mean size of five largest metastases per lung area (right), n = 4 mice in AR+ groups, n = 5 in AR- groups. One-way ANOVA, Šídák’s test. p, H&E staining. Black arrows indicate metastatic lesions. Data are shown as mean ± SEM; box plots show median (Q2), Q1–Q3, and whiskers (min–max).
Extended Data Fig. 3 Proliferative, migratory, and clonogenic behaviour of AR+ and AR- LLC and LMB cells with and without RT.
a, In vitro proliferation of tumour cells treated with recombinant AREG. Proliferation measured as percent of confluency, analysed by live cell imaging over 72 h, n = 3 wells per condition and cell line. b, In vitro horizontal migration after scratch-wound assay of tumour cells treated with recombinant AREG. Migration measured as percent of confluency of wound area, analysed by live cell imaging over 48 h. n = 3 wells per condition and cell line. c, In vitro proliferation of tumour cells treated with RT. Proliferation measured as percent of confluency, analysed by live cell imaging over 72 h. Cells were irradiated with 0, 2, 4, or 6 Gy 24 h before start of proliferation assay. n = 3 wells per condition and cell line. d, In vitro migration of tumour cells measured by transwell assay. 1 × 103 cells were plated in serum-free media in inserts (8.0 µm pore size) overnight. Cells in the mesh were counted as migrating cells (left), images of migrated cells in mesh (right), n = 3 wells per cell line. e, In vitro migration of tumour cells post-RT measured by transwell assay. Tumour cells were irradiated with 0, 2, 4, or 6 Gy. The next day 1 × 103 cells were plated in serum-free media in inserts (8.0 µm pore size) overnight, n = 4 wells per condition and cell line. f, Microscopy images of migrated cells post-RT in mesh. g, In vitro colony formation of tumour cells treated with RT. 100 cells were seeded / well, allowed to attach overnight and then irradiated with 0, 2, 4, 6, or 8 Gy. Colonies containing >50 cells were counted 10 days after seeding, n = 3 wells per condition and cell line. h, In vitro colony formation of AR+ and AR- tumour cells treated with recombinant AREG. Colonies containing >50 cells were counted 10 days after seeding, n = 3 wells per condition and cell line. Panels a-e, g–h representative of at least two independent experiment with similar results. Data are shown as mean ± SEM for a-e and mean for g–h.
Extended Data Fig. 4 Recombinant AREG mimics tumour cell-derived AREG phenotype in vivo.
a, H&E staining of lungs 7 days post i.v. injection of 1 × 105 LLCAR+ and LLCAR− tumour cells. Black arrows indicate metastatic lesions. b, Number of lung metastases (left), and mean size of five largest metastases per lung area (right), n = 4 mice per group. Unpaired two-sided t-test. c, H&E staining of lungs 14 days post i.v. injection of 1 × 105 LLCAR+ and LLCAR− tumour cells. Black arrows indicate metastatic lesions. d, Number of lung metastases (left), and mean size of five largest metastases per lung area (right), n = 4 mice per group. Unpaired two-sided t-test. e, Number of metastases per lung (left) and mean size of largest metastases per lung area after ± intravenous (i.v.) recombinant AREG (rAR) treatment (right), n = 5 in LLCAR+ + rAR group, n = 4 mice in all other groups. One-way ANOVA, Šídák’s test. f, Growth curve of LLC flank tumours ± 20 Gy RT or complete surgical resection of the flank tumour on day 11, 14, and 18, n = 4 mice in 20 Gy, n = 5 in all other groups. g, AREG concentration in serum of tumour-bearing mice five days after 20 Gy RT or complete surgical resection of the flank tumour, measured by ELISA, n = 3 mice in 20 Gy, n = 5 in all other groups. One-way ANOVA, Šídák’s test. h, Number of lung metastases (left - One-way ANOVA, Šídák’s test), and mean size of the five largest metastases per lung area (right – unpaired two-sided t-test), n = 4 mice in 20 Gy, n = 5 in all other groups. i, H&E staining. Black arrows indicate metastatic lesions. j, Dot plot of Gene Set Enrichment Analysis (GSEA) comparing upregulated Hallmark pathways in RNA-seq of LLCAR+ + 4 Gy. k, Volcano plot of up- and downregulated genes in LLCAR+ cells + 4 Gy RT. Significantly upregulated differentially-expressed genes (DEGs) involved in type-I-IFN pathway are coloured in red. DEGs determined by Wald test, Benjamini-Hochberg FDR correction (DESeq2). l, Relative expression of Areg in LLCAR+ cells after interferon β (IFNβ) treatment, measured by RT-qPCR. One-way ANOVA, Dunnett’s test. n = 3 technical repeats. m, AREG concentration in LLCAR+ cells after IFNβ treatment, measured by ELISA. Kruskal-Wallis, Dunn’s test. n = 3 technical repeats. n, Relative expression of Areg in LLC cells post-RT and siSTAT2 treatment, measured by RT-qPCR. One-way ANOVA, Šídák’s test. n = 3 technical repeats. o, AREG concentration in LLCAR+ cells after 4 Gy RT and siSTAT2 treatment, measured by ELISA. One-way ANOVA, Šídák’s test. n = 3 technical repeats. Data are shown as mean ± SEM; box plots show median (Q2), Q1–Q3, and whiskers (min–max).
Extended Data Fig. 5 Extended information about human PBMC and immune cell populations in LLCAR+ and LLCAR− lungs ± RT.
a, Spectral flow cytometry and unsupervised t-SNE clustering of 800,000 live CD45+ PBMCs of n = 30 matched samples (n = 15 patients), pre- and post SBRT. Expression intensity of selected extracellular markers. b, Unsupervised cluster assignment of 25 PBMC clusters (k-nearest neighbours & FlowSOM). c, Heatmap of marker expression across PBMC clusters. Black box highlights CD33+ CD14+ p-EGFR+ monocytes (population 4). d, Spectral flow cytometry and t-SNE clustering of 230,000 live CD45+ immune cells from lungs of non-tumour-bearing (n = 3) and tumour-bearing (n = 5 per group) mice. Expression intensity of selected extracellular markers. e, Unsupervised cluster assignment of 16 murine lung immune cell clusters (k-nearest neighbours & FlowSOM). f, Heatmap of marker expression in murine lung immune cell clusters. Black box highlights Ly6C+, F4/80+, p-EGFR+ monocyte-derived macrophages (population 3). g, t-SNE density plots from lung tissue of non-tumour-bearing (NTB) vs. tumour-bearing mice, myeloid and adaptive immune cell clusters are outlined. h, Heatmap of immune cell populations identified by surface marker expression using conventional gating, after max normalization of the fraction of live CD45+ cells. Asterisk: highest fraction of Ly6C+, F4/80+ population. i, Quantification of CD8+ and CD4+ T cells and CD19+ B cells in the lung tissue of LLCAR+ and LLCAR− ± 20 Gy tumour-bearing mice, identified by surface marker expression using conventional gating, normalized per mg lung tissue, n = 5 mice per group. One-way ANOVA, Šídák’s test. j, Schematic overview of workflow for AI-based cell segmentation model followed by logistic regression classifier training. DAPI nuclear stain= blue, Tyr992 p-EGFR = AF488 (green), Ly6C = PE/Dazzle 594 (red). k, Confusion matrix showing the performance of the classification model. AUC = area under the curve. Box plots in i show median (Q2), Q1–Q3, and whiskers (min–max).
Extended Data Fig. 6 Extended information about immune populations identified by scRNA-seq in LLCAR+ and LLCAR lungs ± 20 Gy.
a, Unsupervised uniform manifold approximation and projection (UMAP) of 32,690 live CD45+ cells in the lungs of LLCAR+ and LLCAR− tumour-bearing mice ± 20 Gy, n = 4 mice per group, annotated into 11 major cell lineages. Conv. type I DC = conventional type I dendritic cells, Alv. Mac = alveolar macrophages, Treg = regulatory T cells, NK cell = natural killer cells, ILC2 = group 2 innate lymphoid cells. b, UMAP of CD45+ cells stratified by condition; monocytes, B cells, T cells, NK cells, and neutrophils are outlined. c, t-SNE projection of the global transcriptomic profile from 16 individually hashtagged mice across four conditions. d, Bubble plot showing the top three marker differentially expressed genes (DEGs) for 11 major cell lineages. DEGs identified by two-sided Wilcoxon rank-sum test. e, Volcano plot of DEGs in monocytes from LLCAR+ + 20 Gy. Selected genes are coloured by function. P-values of 0 are depicted at 1−50 (log10). Two-sided Wilcoxon rank-sum test. f, Volcano plot of DEGs in monocytes from LLCAR− + 20 Gy. Selected genes are coloured by function. Two-sided Wilcoxon rank-sum test. g, UMAP of MNPs stratified by experimental condition. Monocytes, conv. type I DCs, plasmacytoid DCs, migratory DCs, and alveolar macrophages are outlined. Annotations assigned using Pegasus auto-annotation and top DEGs. Alv_mac = alveolar macrophage, cDC1 = conventional type 1 DC, pDC = plasmacytoid DC. Cluster colours consistent with Fig. 3c. h, Dot plot and bar graph showing the fraction of cells in 17 MNP subclusters across conditions. Mono = monocyte, Alv_macro = alveolar macrophage, Plasm_DC = plasmacytoid DC, Mo_DC = monocyte-derived DC, Int_macro = interstitial macrophage, Migr_DC = migratory DC, Class_DC_1 = classical type 1 DC. i, Volcano plot of DEGs in population 1 (Mono_Fn1). Selected genes are coloured by function. P-values of 0 are depicted at 1−50 (log10). Two-sided Wilcoxon rank-sum test.
Extended Data Fig. 7 Extended information about pseudotime and trajectory analysis of monocytes identified by scRNA-seq.
a, UMAP of 4,095 MNPs from lungs of LLCAR+ and LLCAR− tumour-bearing mice ± 20 Gy, n = 4 mice per group. Clusters used for pseudotime analysis (2,600 monocytes) outlined. Cluster colours and names consistent with Fig. 3c. b, Heatmap of top differentially expressed genes (DEGs) of the seven monocyte populations used for trajectory analysis. c, Violin plot of pseudotime values for 2,600 monocytes, stratified by experimental condition. d, Violin plot of pseudotime values across seven monocyte subpopulations. e, Frequency of cells from the four experimental groups in population 1. f, Heatmap of Reactome pathways related to EGFR signalling in population 1 vs. all other populations. g, Frequency of cells from four experimental conditions in Pop3 Mono_ S100a9 and Pop7 Mono_Adgre4. h, Volcano plot of DEGs in populations 3 and 7, selected genes coloured by function. P-values of 0 are depicted at 1−50 (log10). Two-sided Wilcoxon rank-sum test. i, Pie chart of total monocyte RNA splicing ratios detected by scVelo. j, Bar plot of splicing ratios across seven monocyte populations. k, Phase portraits of unspliced vs. spliced RNA ratios for Thbs1 and Clec4e (first and last gene in l). Right: inferred velocity and gene expression projected onto diffusion map. l, Time-series heatmap of the top forty velocity-informed driver genes visualized across trajectory monocyte clusters, ordered by diffusion pseudotime. m, Volcano plot of DEGs in trajectories 1 and 2, selected genes coloured by function. P-values of 0 are depicted at 1−50 (log10). Two-sided Wilcoxon rank-sum test. n, Expression of selected genes involved in antigen processing and presentation, phagolysosomal processes and immunosuppression, projected onto the diffusion map. o, Heatmap of Reactome pathway enrichment in trajectories 1 and 2 related to antigen processing and presentation, inflammation, and EGFR signalling.
Extended Data Fig. 8 AREG induces T-cell suppressive monocyte phenotype, but T cells do not determine lung metastasis in vivo.
a, Heatmap of individual genes and overall gene signature genes involved in immunosuppression in monocyte cluster from Fig. 3a. b, Heatmap of individual genes and overall gene signature of terminal T-cell exhaustion (Miller et al.31) in CD8+ T cell cluster 2 from Fig. 3a. c, Experimental setup: BMDM from Egfrflx/flx (EGFR + ) and LysMΔEgfr (EGFR-) mice were co-cultured with LLCAR+ or LLCAR− tumour cells followed by fluorescence-activated cell sorting (FACS) of Ly6C+ cells and RNA-seq (n = 3 technical replicates). Created in BioRender. Piffkó, A. (2025) https://BioRender.com/s42t906. d, Dot plot of Gene Set Enrichment Analysis (GSEA) showing upregulated Hallmark pathways in conditions 2 vs. 1 (LLCAR− + EGFR+ MNPs vs. LLCAR+ + EGFR+ MNPs). Wald test and Benjamini-Hochberg method. e, Dot plot of GSEA showing upregulated Hallmark pathways in conditions 4 vs. 3 (LLCAR− + EGFR- MNPs vs. LLCAR+ + EGFR- MNPs). Wald test and Benjamini-Hochberg method. f, Heatmap of normalized counts of genes involved in cell killing (RNA-seq of Ly6C+ MNPs; gene signatures in f-h adapted from Wang et al.29). g, Heatmap of genes related to reactive oxygen species (ROS) biosynthetic processes in Ly6C+ MNPs. h, Heatmap of phagocytosis-related genes in Ly6C+ MNPs. i, Heatmap of immunosuppressive genes in Ly6C+ MNPs. j, Proliferation of CD8+ T cells after co-culture with bone-marrow derived myeloid cells (BMDM) pre-treated with rAR (left), and histogram of proliferating CD8+ T cell populations (right), n = 3 technical replicates. One-way ANOVA, Šídák’s test. k, Growth curves of LLCAR+ and LLCAR− flank tumours ± i.v. CD8-antibody (αCD8), n = 7 mice in AR+ groups, n = 6 in LLCAR−, n = 8 in LLCAR− + αCD8. Two-way ANOVA, Tukey’s test. l, Number of metastases (left), and size of five largest metastases per lung area post-αCD8 treatment (right), n = 5 mice in AR+ groups, n = 4 mice in AR- groups. One-way ANOVA, Šídák’s test. m, H&E staining. Black arrows indicate metastatic lesions. Data is shown as mean ± SEM; box plots show median (Q2), Q1–Q3, and whiskers (min–max).
Extended Data Fig. 9 Anti-CCR2 antibody-mediated depletion of MNPs determines in vivo lung metastasis phenotype.
a, Count of CD11b+ Ly6C+ monocytes, CD11b+ F4/80+ macrophages, CD11c+ MHCII+ dendritic cells, CD11b+ Ly6G+ granulocytes, and CD11b- SiglecF+ alveolar macrophages per μg lung tissue in LLC tumour-bearing mice treated with anti-CCR2 antibody (αCCR2), n = 5 mice per group. Populations identified using conventional gating strategy. Unpaired two-sided t-test. b, Number of lung metastases (left), and mean size of the five largest metastases per lung area (right) of LLCAR+ + αCCR2, n = 7 mice LLCAR+, n = 6 mice αCCR2. Unpaired two-sided t-test for number and two-sided Mann-Whitney test for size. c, H&E staining. Black arrows indicate metastatic lesions. d, Number of lung metastases (left), and mean size of the five largest metastases per lung area (right) of LLCAR− + αCCR2, n = 8 mice LLCAR−, n = 7 mice αCCR2. Unpaired two-sided t-test. e, H&E staining. Black arrows indicate metastatic lesions. Box plots show median (Q2), Q1–Q3, and whiskers (min–max).
Extended Data Fig. 10 AREG upregulates CD47 via STAT3 signalling to suppress MNP phagocytosis.
a, Schematic of live cell imaging co-culture system with CellTracker Red tumour cells and CellTracker Green bone-marrow derived myeloid cells (BMDM) (top). Fraction of engulfed LLCAR+ and LLCAR− tumour cells after 4 h, n = 10 technical replicates (bottom). Created in BioRender, Piffkó A, 2025. https://biorender.com/t54k444. b, Live cell imaging of co-culture system with CellTracker labelled tumour cells and BMDMs. c, Cd47 expression in LLCAR+ (left) and LLCAR− post-RT (right), measured by RT-qPCR, n = 2 technical replicates. d, Histogram and quantification of CD47 mean fluorescence intensity (MFI) on LLCAR+ and LLCAR− cells ± 4 Gy, n = 2 technical repeats. e, MFI of p-STAT3 (Tyr705) in LLC cells, after 25 min of rAR treatment at indicated concentrations, n = 3 technical replicates. One-way ANOVA, Šídák’s test. f, Cd47 expression in LLCAR+ cells post-rAR treatment, measured by RT-qPCR, n = 2 technical replicates. g, Cd47 expression in LLCAR+ cells post-RT, rAR, and STAT3i (Stattic, 5 μM) treatment, measured by RT-qPCR, n = 2 technical replicates. h, IF staining of Ly6C+ MNPs co-cultured with LLC tumour cells, stained for MyoIIA (AF488, green) and CD47 (BV421, blue). Close-up of phagocytic synapse. i, IF staining of Ly6C+ MNPs co-cultured with LLCAR+ (left) and LLCAR− (right). Stained for p-MyoIIA (AF488, green), Ly6C (PE/Dazzle 594, red), and CD47 (BV421, blue). Data are shown as mean ± SEM. One representative experiment out of two independent experiments is shown.
Extended Data Fig. 11 AREG blockade synergizes with anti-CD47 and increases MNP phagocytosis in vivo.
a, Kaplan-Meier plot of progression-free survival stratified by AREG serum levels, measured by ELISA. n = 42 samples from n = 21 patients (pre-SBRT and after three cycles of ICB + SBRT). Log-rank (Mantel-Cox) test. b, Representative gating strategy for mouse lung tissue identifying RFP+ phagocytic MNP populations. c, Percentage of phagocytic RFP + Ly6C+ monocytes (left), RFP + Ly6G+ neutrophils, RFP + CD11c+ MHCII+ dendritic cells, and RFP+ CD11b- Siglec-F+ alveolar macrophages shown as percentage of the parent population. Cells isolated from lungs of LLCAR+ tumour-bearing mice that were treated with 20 Gy RT or a combination with anti-AREG- (αAR) and anti-CD47-antibody (αCD47). n = 5 in LLCAR+ and 20 Gy group, n = 6 in other groups. One-way ANOVA, Šídák’s test. Box plots show median (Q2), Q1–Q3, and whiskers (min–max).
Extended Data Fig. 12 Tyr992 p-EGFR expression of Ly6C+ MNPs from lung tissue of LLCAR+ tumour-bearing mice treated with 20 Gy RT, αAR, and αCD47.
a, Percentage of CD11b+ Ly6C+ MNPs, CD11b− SiglecF+ alveolar macrophages and CD3+ CD8+ T cells, shown as percentage of live CD45+ cells from lungs of LLCAR+ tumour-bearing mice treated with 20 Gy RT, anti-AREG-antibody (αAR), and anti-CD47-antibody (αCD47). n = 6 mice per group. One-way ANOVA, Šídák’s test. b, t-SNE dimensionality reduction of 250,000 live CD45+ immune cells from lung tissue. c, Expression intensity of extracellular markers projected onto t-SNE. d, Identification of 16 immune cell populations by unsupervised clustering (k-nearest neighbours & FlowSOM). e, Expression intensity of Tyr992 p-EGFR projected onto t-SNE. f, Identification of two clusters with the highest p-EGFR expression (Clusters 13 and 15). g, Heatmap of marker expression across 16 clusters. Black boxes highlight MNP populations with high expression of Tyr992 p-EGFR (populations 13 and 15). h, Density plot of t-SNEstratified by experimental condition; p-EGFR+ MNP populations outlined. i, Percentage of p-EGFR+ MNP populations, shown as percentage of live CD45+ cells, n = 5 mice per group. One-way ANOVA, Šídák’s test. Box plots show median (Q2), Q1–Q3, and whiskers (min–max).
Supplementary information
Supplementary Table 1
Characteristics of clinical cohort shown in Fig. 1a,b and Extended Data Fig. 1b (tissue biopsies pre- and post SBRT)
Supplementary Table 2
List of 60 genes induced post-SBRT correlating with progression of distant metastatic lesions based on RECIST scoring, shown in Fig. 1a.
Supplementary Table 3
Characteristics of clinical cohort shown in Fig. 2a–f and Extended Data Fig. 5a–c (spectral flow of PBMCs) and in Extended Data Fig. 11a (serum ELISA).
Supplementary Table 4
Lists of differentially expressed genes (DEGs) that are up- and downregulated in 21 CD45+ clusters identified by scRNA-seq, shown in Fig. 3a.
Supplementary Table 5
Lists of DEGs that are up- and downregulated in 17 MNP clusters identified by scRNA-seq, shown in Fig. 3c.
Source data
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Piffkó, A., Yang, K., Panda, A. et al. Radiation-induced amphiregulin drives tumour metastasis. Nature (2025). https://doi.org/10.1038/s41586-025-08994-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41586-025-08994-0



