Abstract
Observational studies indicate that serum sex hormone-binding globulin (SHBG) levels are inversely correlated with blood lipid levels and coronary heart disease (CHD) risk. Given that dyslipidemia is an established risk factor for CHD, we aim to employ Mendelian randomization (MR) in conjunction with mediation analysis to confirm the mediating role of blood lipid levels in the association between SHBG and CHD. First, we assessed the causality between serum SHBG levels and five cardiovascular diseases using univariable MR. The results revealed causality between SHBG levels and reduced risk of CHD, myocardial infarction, as well as hypertension. Specifically, the most significant reduction was observed in CHD risk, with an odds ratio of 0.73 (95% CI 0.63–0.86) for each one-standard-deviation increase in SHBG. The summary-level data of serum SHBG levels and CHD are derived from a sex-specific genome-wide association study (GWAS) conducted by UK Biobank (sample size = 368,929) and a large-scale GWAS meta-analysis (60,801 cases and 123,504 controls), respectively. Subsequently, we further investigated the mediating role of blood lipid level in the association between SHBG and CHD. Mediation analysis clarified the mediation proportions for four mediators: high cholesterol (48%), very low-density lipoprotein cholesterol (25.1%), low-density lipoprotein cholesterol (18.5%), and triglycerides (44.3%). Summary-level data for each mediator were sourced from the UK Biobank and publicly available GWAS. The above results confirm negative causality between serum SHBG levels and the risk of CHD, myocardial infarction, and hypertension, with the causal effect on reducing CHD risk largely mediated by the improvement of blood lipid profiles.
Similar content being viewed by others
Introduction
Sex hormone-binding globulin (SHBG) is a circulating plasma protein synthesized by liver cells. Traditional perspectives suggest that its primary physiological function is to regulate the bioavailability and metabolic clearance of sex hormones by specifically binding to them. It can also exert direct biological effects on tissues and cells dependent on sex hormones1. However, in recent years, in-depth research on SHBG has generated new insights, suggesting that it is closely associated with metabolic-related phenotypes and diseases such as blood lipids, hepatic fat content, obesity, insulin resistance, and diabetes2,3,4,5. Previous research has indicated association between higher serum SHBG levels and favorable lipid profile6,7,8, but traditional observational studies are susceptible to various biases9. Therefore, these findings need to be further verified by evidence-based medicine methods with higher level of evidence. Additionally, other studies have shown inverse association between serum SHBG levels and the risk of coronary heart disease (CHD)10, but the mechanism is not clear. The lipid infiltration hypothesis is currently the most widely accepted theory explaining the mechanism of atherosclerosis11. Of course, not only this process involves lipid accumulation, but also molecular processes such as excessive inflammatory response play an important role12. Therefore, dyslipidemia has been considered to be one of the most important risk factors for CHD13. In light of this, it is reasonable to speculate that the improvement of lipid profiles may play a crucial mediating role in the association between SHBG and CHD, and this hypothesis can be validated through joint mediation analysis.
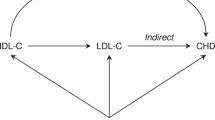
Mendelian randomization (MR) is a novel causal inference method that has been increasingly employed in recent years. Its fundamental principle involves using genetic variation as instrumental variables (IVs) to predict the corresponding exposure. If populations with these genetic variations exhibit higher occurrence of the relevant outcome, it can establish a causality between exposure and outcome14. Since individual genetic variations are randomly allocated at conception and not influenced by postnatal factors, MR can overcome issues of confounders and reverse causality commonly encountered in traditional observational studies15. Additionally, when traditional epidemiological studies are costly and exposure are difficult to measure, MR can serve as a valuable technique15. Of course, this method has some limitations. The use of genetic variations as IVs in MR studies must satisfy three core instrumental variable (IV) assumptions: the relevance assumption, independence assumption, and exclusion restriction assumption (Fig. 1A)16. Because the IV assumptions are difficult to be fully verified, MR must be used with caution for causal inference. If these three assumptions are not entirely met, the analysis results may be subject to bias16.
Overview of this study and illustrative diagram of the MR core IV assumption. (A) The illustrative diagram of three core instrumental variable assumptions in MR, with the incorporation of the mediators relevant to this study. (B) X, Y and Z represent exposure, mediator, and outcome, respectively. βXY and βXZ are derived using UVMR, while β*XY and βZY are derived using MVMR with mutual adjustments for SHBG and mediator. (C) The study process is divided into four stages, corresponding to the "Study design and process" section. SHBG sex hormone-binding globulin, CHD coronary heart disease, CVDs cardiovascular diseases, MR Mendelian randomization, UVMR univariable Mendelian randomization, MVMR multivariable Mendelian randomization, IV instrumental variable, SNPs single-nucleotide polymorphisms.
Using MR, we aimed to further investigate the causality of serum SHBG levels on blood lipid levels and CHD risk. Mediation analysis was also introduced to demonstrate the mediating role of blood lipid levels in the causality between serum SHBG levels and CHD, and to determine the mediation proportion.
Methods
Study design and process
First, using univariable Mendelian randomization (UVMR) to assess the causality between serum SHBG levels and five cardiovascular diseases (CVDs), it was found that SHBG has the most significant causality with a reduced risk of CHD. Consequently, further research was conducted to investigate whether SHBG affects CHD through mediator (blood lipid levels). Second, we conducted bidirectional UVMR between serum SHBG levels and blood lipid levels, as well as between blood lipid levels and CHD. If there is a potential reverse causality, we employed the Steiger directionality test to assess the validity of the forward causality17. Subsequently, we performed multivariable Mendelian randomization (MVMR) with adjustment for SHBG to evaluate the direct effect of blood lipid levels on CHD. Third, we calculate the mediation proportion using the product method18,19. When there was sample overlap between the genome-wide association study (GWAS) on exposure and the GWAS on mediator, we then employ the difference method to compute the mediation proportion18. Fourth, conduct sex-specific analysis. The entire study design and process are illustrated in the Fig. 1B,C. This study strictly adheres to the reporting guidelines of Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization (STROBE-MR)20,21.
This study uses publicly available GWAS summary-level data, and thus, ethical approval is not required. Ethical approval and participant informed consent for the original GWAS can be found in the referenced GWAS publications and in the official websites of the respective databases.
Data sources
The summary-level data stratified by gender for serum SHBG levels were derived from the largest sex-specific GWAS conducted by the UK Biobank, with BMI adjustments. This GWAS was also replicated in three independent studies (CHARGE Consortium, Twins UK and EPIC-Norfolk)22. The summary-level data of total cholesterol (TC) were obtained from 23 studies conducted by the Global Lipids Genetics Consortium, involving 94,595 participants of European ancestry23. The summary-level data of triglycerides (TG) and high density-lipoprotein cholesterol (HDL-C) were obtained from a GWAS conducted by the Within Family Consortium in 202224. We acquired these data from the IEU OpenGWAS project (https://gwas.mrcieu.ac.uk/datasets), with the GWAS IDs being ieu-b-4850 and ieu-b-4844, respectively. Within Family GWAS can significantly mitigate the false genetic variation-phenotype association bias induced by transmission ratio distortion, population stratification, and assortative mating, thus providing more reliable causal effect estimates25. The summary-level data of low density-lipoprotein cholesterol (LDL-C) were derived from a GWAS involving 431,167 individuals from the UK Biobank26. The summary-level data of very low density-lipoprotein cholesterol (VLDL-C) were obtained from a GWAS conducted by Nightingale Health on 500,000 plasma samples from the UK Biobank27. The summary-level data for high cholesterol and hypercholesterolemia were obtained through the analysis of the UK Biobank genetic dataset using the GWAS pipeline developed by the Medical Research Council Integrative Epidemiology Unit at the University of Bristol28. This pipeline includes steps such as data quality control, genotype preprocessing, phenotype preprocessing, association analysis, and result integration28. The summary-level data of CHD were obtained from a large-scale GWAS meta-analysis conducted by the CARDIoGRAMplusC4D consortium, involving 48 studies and a total of 184,305 participants29. The summary-level data of myocardial infarction (MI) were derived from a subgroup analysis of this GWAS meta-analysis, accounting for approximately 70% of the total cases29. The summary-level data of hypertension, heart failure, and atrial fibrillation and flutter were all obtained from the FinnGen consortium R9 release30. The Finnish consortium defines these diseases using the codes from the International Classification of Diseases 8th, 9th, and 10th editions.
All details regarding the GWAS summary-level data and related databases mentioned above can be found in the Supplementary Tables S1–S4 and Supplementary Methods S1. The units for GWAS summary-level data across all phenotypes, the utilized regression models, and statistical transformations applied to certain data, are reported in the Supplementary Methods S2.
Genetic instruments selection
The IVs [i.e., single nucleotide polymorphisms (SNPs)] associated with SHBG, blood lipid levels, and CVDs will be selected through the following steps. First, SNPs need to reach the genome-wide significance threshold (P < 5 × 10–8). Second, SNPs must be independent of each other, and we set the threshold for linkage disequilibrium as r2 < 0.001 and clumping window > 10,000 kb. Third, we also calculated the F-statistic for each SNP to assess their strength of association with the phenotype, and SNPs with an F-statistic less than 10 will be considered weak IVs and excluded31. The F-statistic is calculated as follows: \(F=N\times \frac{{R}^{2}}{1-{R}^{2}}\), where R2 is the variability explained by each SNP, and N is the GWAS sample size32. To calculate R2 for the extended 10 SNPs, we used the following formula: \({R}^{2}=\frac{{\beta }^{2}}{{\beta }^{2}+N\times {SE}^{2}}\), where β is the estimated genetic effect and SE is the standard error of the genetic effect33. Before conducting MR analysis, all datasets need to be harmonized to align the direction of the allele of the SNPs associated with exposure and outcome and to exclude palindromic and inappropriate SNPs.
UVMR and MVMR analysis
We conducted UVMR to assess the total causal effect of SHBG on five CVDs. Additionally, we performed bidirectional UVMR to evaluate the reciprocal causal effects among SHBG, blood lipid levels, and CHD. Furthermore, we conducted sex-specific analysis of the causality between SHBG and CHD using sex-stratified summary-level data. Inverse variance weighted (IVW) method is used as the primary UVMR analysis method, and the choice of the analytical model depends on the heterogeneity situation. This method is the meta-analysis of Wald ratios for each SNP34, thus providing the most accurate estimate of causal effects. However, it assumes that all IVs are valid, making it susceptible to potential horizontal pleiotropy35,36. Therefore, we employed the weighted median, MR-Egger, and MR-Pleiotropy Residual Sum and Outlier (MR-PRESSO) method as supplementary analytical methods. The weighted median method provides consistent estimates of causal effects when at least 50% of the weight comes from valid IVs37. The MR-Egger method can detect the presence of pleiotropy in MR analysis results and provide effect estimates that are not influenced by violations of IV assumptions38,39. The MR-PRESSO method can detect potentially pleiotropic SNPs (i.e., outliers) and assess whether removing outliers affects the effect estimates40. We further assessed the direct effects of SHBG and blood lipid levels on the CHD after mutual adjustment using MVMR18, with the IVW being the sole analytical method.
For continuous outcomes, the results will be presented using regression coefficient (i.e., β) and their 95% confidence interval (CI). For dichotomous outcomes, the main results will be reported in terms of odds ratio (OR) and its 95% CI.
Mediation MR analysis
We employed a two-step MR to assess whether blood lipid levels act as mediators in mediating the risk reduction of CHD associated with SHBG. The two-step MR produced the following four effect estimates: (1) The total effect of SHBG on CHD (βXY); (2) The total effect of SHBG on the mediators (βXZ); (3) The direct effect of SHBG on CHD (β*XY); (4) The effect of mediators on CHD adjusting for SHBG (βZY) (Fig. 1B). The indirect effect was calculated using the coefficient product method: Indirect effect = βXZ × βZY. And the mediation proportion was computed by dividing the indirect effect by βXY18,19. When there was sample overlap between the GWAS on exposure and the GWAS on mediators, the indirect effect can be calculated using the difference method: Indirect effect = βXY − β*XY18. Because this method does not require the effect estimates of exposure on mediators, the resulting indirect effect is theoretically unaffected by the bias introduced by sample overlap. Next, we compare the mediation proportions calculated using the two methods. The 95% CI for mediation proportion are calculated using the delta method41 and bootstrap method.
Sensitivity analyses
MR-Egger intercept test was used to detect potential horizontal pleiotropy in the results of UVMR39, while the Cochran's Q test was used to assess heterogeneity. When the p-values calculated by these two methods are less than 0.05, it indicates the presence of pleiotropy and heterogeneity, respectively. If horizontal pleiotropy is absent, it can provide evidence for the validity of assumption III. Considering the possibility of reverse causality and its impact on the reliability of the results, we used the Steiger directionality test to validate the validity of the forward causality17. Due to concerns that sample overlap between exposure and mediators may inflate causality and increase type I error rates42, we used MRlap to correct for bias caused by sample overlap43, and evaluated its impact on the results (Supplementary Methods S3). We used MR visualization methods to visually present the results of the UVMR. The scatter plot depicted the effect estimates and intercept of the MR-Egger method, while the funnel plot displayed heterogeneity. Additionally, leave-one-out analysis was conducted to assess the robustness of the results. In the MVMR analysis, we employed the "pleiotropy_mvmr" and "strength_mvmr" functions from the "MVMR" package to assess heterogeneity and the overall F-statistic for individual variable's SNPs, respectively.
Based on the aforementioned methods, the MR analysis results are defined as having a significant causality only if the following conditions are met: (1) The p-value of the IVW method is less than 0.05; (2) The effect estimates from all four MR analysis methods show consistent directions; (3) The MR-Egger intercept test suggests the absence of horizontal pleiotropy; (4) The Steiger directionality test confirms the establishment of forward causality.
In our study, we utilized R packages “TwoSampleMR,” “MRPRESSO,” “MRlap” and “MVMR” in R software version 4.2.2 (https://www.r-project.org/) for all statistical analyses. All p values in this study are two-sided, and the statistical significance was set at < 0.05.
Ethics declarations
The ethical approval and informed consent from participants for the original GWAS are available in the cited GWAS publications and on the official websites of the relevant databases.
Results
Genetic instruments
The detailed information for genetic IVs used in UVMR and MVMR, along with their F-statistics, is reported in Supplementary Table S5–S25. All F-statistics are greater than 10, indicating the absence of weak instrument bias. Since less than 20% of the IVs were missing in the outcome summary-level data (except for TC), we did not search for proxy SNPs.
Effects of SHBG on multiple CVDs
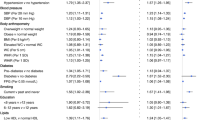
We conducted initial analysis of the causality between SHBG and five CVDs. The IVW method indicates that each increase of one-standard-deviation (1-SD) in SHBG is associated with a reduced risk of CHD (OR 0.73; 95% CI 0.63–0.86), MI (OR 0.77; 95% CI 0.66–0.90), and hypertension (OR 0.84; 95% CI 0.74–0.96), but not with the other two CVDs (Fig. 2). The results of the other three MR analysis methods can be found in Supplementary Fig. S1. The MR-Egger intercept test did not detect horizontal pleiotropy, but all results exhibited varying degrees of heterogeneity (Supplementary Table S26). Since the association between SHBG and CHD is the most significant, we proceeded with the subsequent mediation analysis for this outcome.
Effects of SHBG on blood lipid levels and CHD
In the UVMR analysis, the IVW method indicates that each increase of 1-SD in SHBG is associated with a decrease in LDL-C (β = − 0.112; 95% CI − 0.220 to − 0.003), VLDL-C (β = − 0.245; 95% CI − 0.347 to − 0.144), and TG (β = − 0.487; 95% CI − 0.602 to − 0.373) levels, and an increase in HDL-C (β = 0.353; 95% CI 0.243–0.463) levels (Fig. 3). The unit for all effect estimates (i.e., β) is 1-SD. Furthermore, the IVW method also indicates that each increase of 1-SD in SHBG is associated with a reduced risk of high cholesterol (OR 0.72; 95% CI 0.64–0.82), hypercholesterolemia (OR 0.71; 95% CI 0.61–0.82), and CHD (OR 0.73; 95% CI 0.63–0.86) (Fig. 4). The direction of the effect estimates in the other three MR analysis methods is consistent with the IVW method. The MR-Egger intercept test detected horizontal pleiotropy in the MR analysis results of SHBG on HDL-C (intercept = 2.30 × 10–3; p-value = 0.04), and all results exhibited varying degrees of heterogeneity (Table 1). However, funnel plots of all results appear relatively symmetric, showing no pronounced heterogeneity or pleiotropy, while scatter plots offer a more intuitive presentation of the results in an alternative format (Supplementary Figs. S2-S9).
Mendelian randomization analysis to estimate the causal effects of SHBG levels on five continuous phenotypes. SHBG sex hormone-binding globulin, HDL-C high-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol, VLDL-C very low-density lipoprotein cholesterol, TG triglycerides, TC total cholesterol, SNPs single-nucleotide polymorphisms, CI confidence interval.
The IVW method of the reverse MR analysis indicates a reverse causality between SHBG and CHD, TG, HDL-C, VLDL-C, as well as high cholesterol, but the effect estimates and/or significance of the association are considerably lower than the forward causality (Supplementary Table S27). Corresponding sensitivity analysis reveals significant heterogeneity in all results, and MR-Egger intercept test indicates the presence of horizontal pleiotropy in the reverse MR analysis results between SHBG and HDL-C (intercept = 3.66 × 10–3; p-value = 0.02) (Supplementary Table S28). The results of the Steiger directionality test indicate that the direction of the causal effects of SHBG on mediators and CHD is true, and the directionality tests are all significant (p < 0.05).
Therefore, the directionality of the forward causality between SHBG and CHD, as well as all mediators, is established (Table 2). We also used MRlap to correct for the bias caused by sample overlap between SHBG and LDL-C, VLDL-C, high cholesterol, as well as hypercholesterolemia, and there were no significant differences in effect estimates and significance of the association before and after correction (Supplementary Table S29).
Taking into account the results from the above analysis, based on the previously established definition of significant causality, the causality between SHBG and CHD, high cholesterol, hypercholesterolemia, LDL-C, VLDL-C, as well as TG are established.
Effects of blood lipid levels on CHD
In the UVMR analysis of mediators and CHD, the IVW method indicates that each increase of 1-SD in LDL-C, VLDL-C, TG, and TC is associated with an increased risk of CHD. High cholesterol and hypercholesterolemia are also associated with an increased risk of CHD, while each increase of 1-SD in HDL-C is associated with a reduced risk of CHD (Supplementary Fig. S10). The MR-Egger intercept test detected horizontal pleiotropy in the MR analysis results of TC on CHD, and all results exhibited varying degrees of heterogeneity (Supplementary Table S30). All funnel plots and scatter plots for the MR analyses can be found in Supplementary Fig. S11–S17. For some of the analysis results, we also constructed forest plots of individual SNPs and conducted leave-one-out analysis (Supplementary Fig. S15–S17).
The IVW method of the reverse MR analysis indicates a reverse causality between CHD and LDL-C, high cholesterol, as well as hypercholesterolemia (Supplementary Table S27). Corresponding sensitivity analysis reveals significant heterogeneity in all results, and MR-Egger intercept test did not detect horizontal pleiotropy (Supplementary Table S28). The results of the Steiger directionality test indicate that the direction of the causal effects of mediators on CHD is true, and most directionality tests are significant (p < 0.05) except for the result of hypercholesterolemia (p = 0.878). Therefore, except for hypercholesterolemia, the directionality of the forward causality between mediators and CHD is established (Table 2).
Similarly, based on our established definition of significant causality, the causality between the 6 mediators (high cholesterol, HDL-C, LDL-C, VLDL-C, TG, as well as TC) and CHD are established.
Mediation by blood lipid levels
The MVMR analysis provided direct effects of SHBG and blood lipid levels on CHD. Even after adjusting for SHBG, the causality between all mediators and CHD persists. Every increase of 1-SD in LDL-C (OR 1.67; 95% CI 1.57–1.78), VLDL-C (OR 1.37; 95% CI 1.26–1.49), and TG (OR 1.32; 95% CI 1.20–1.46) is associated with an increased risk of CHD. High cholesterol (OR 1.58; 95% CI 1.48–1.69) and hypercholesterolemia (OR 1.61; 95% CI 1.49–1.74) are also associated with an increased risk of CHD, while each increase of 1-SD in HDL-C (OR 0.84; 95% CI 0.78–0.91) is associated with a reduced risk of CHD (Fig. 5). Except for hypercholesterolemia (F-statistic = 3.8), all variables in the MVMR analysis exhibit sufficient IV strength; all MVMR analysis results exhibit varying degrees of heterogeneity (Supplementary Table S31).
Multivariable Mendelian randomization to assess the direct effects on CHD. Multivariable Mendelian randomization involves mutual adjustment for serum SHBG levels and blood lipid levels. SHBG sex hormone-binding globulin, CHD coronary heart disease, HDL-C high-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol, VLDL-C very low-density lipoprotein cholesterol, TG triglycerides, HCL hypercholesterolemia, OR odds ratio, CI confidence interval.
We conducted a mediation analysis for the causality between SHBG and CHD using the effect estimates obtained. The delta method was the main approach for calculating 95% CI of mediation proportion. The mediation proportions for high cholesterol (48.0%; [95% CI 28.5–68.7%]), VLDL-C (25.1%; [95% CI 13.6–38.6%]), LDL-C (18.5%; [95% CI 0.6–37.0%]), and TG (44.3%; [95% CI 26.6–64.8%), as well as the necessary effect estimates, are shown in Fig. 6. Additionally, we also calculated 95% CI of mediation proportion using the Bootstrap method (Supplementary Fig. S18). The mediation proportion calculated by the difference method can be found in Supplementary Fig. S19.
Mediating effect of blood lipid levels in the causality between SHBG and CHD. 95% CI for the mediation proportion calculated using the delta method. SHBG sex hormone-binding globulin, CHD coronary heart disease, CI confidence interval, VLDL-C very low-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol, TG triglycerides, se standard error.
The sex-specific causality between SHBG and the risk of CHD
The IVW method reveals that with each increase of 1-SD in SHBG, the reduction in CHD risk is greater in the females (OR 0.71; 95% CI 0.61–0.82; p-value = 8.23 × 10–6) compared to the males (OR 0.78; 95% CI 0.66–0.92; p-value = 3.37 × 10–3), and the significance of this association is also greater in females than in males (Fig. 7). However, the MR analysis results exhibit pleiotropy and heterogeneity (Supplementary Table S32). The results from MR-PRESSO with outliers removed may be relatively more accurate, but overall, the obtained results are considered to be unreliable.
Discussion
This MR study demonstrates negative causality between genetically predicted serum SHBG levels and the risk of CHD, MI, as well as hypertension. We found that the causal effect of reducing CHD risk is largely achieved through improving lipid profiles, and we have identified the proportions mediated by blood VLDL-C, LDL-C, TG levels, and high cholesterol.
A meta-analysis incorporating ten previous observational studies indicates that circulating SHBG levels are associated with lower CHD risk in both men and women10. Furthermore, the results of two recent MR studies on the same topic also support the conclusion that an increase in SHBG levels is associated with a reduced risk of CHD10,44. Our mediation analysis highlights that this biological effect of SHBG is largely achieved by improving the blood lipid profiles.
As early as the 1990s, studies had already revealed the association between SHBG and blood lipid levels, primarily limited to the finding of an inverse correlation between SHBG and HDL-C, without elucidating its relationship with other lipid components45,46. Two subsequent cross-sectional studies involving healthy men indicated that low SHBG is associated with an atherogenic lipid profile (low HDL, high VLDL, and high TG); higher SHBG concentrations are related to lower TC, TG, and higher HDL-C8,47. However, given the substantial differences in reproductive endocrinology between males and females, the levels and physiological effects of SHBG may be different between the two groups, and the gender limitation makes it difficult to generalize the conclusions of this study to the entire population. However, a recent cross-sectional study involving 3231 postmenopausal women reported similar results. The serum SHBG levels in the second to fourth quartiles were positively correlated with HDL-C and inversely correlated with non-HDL-C and TG6. Furthermore, a large cohort study conducted by Elif et al., involving 3264 men and women, also indicated an inverse correlation between serum TG and SHBG7. The accumulating body of related research has progressively substantiated the role of SHBG in lipid improvement, with the evidence regarding the correlation between SHBG and HDL-C being the most substantial. Unfortunately, our findings in this regard are subject to horizontal pleiotropy, making it impossible to establish a definitive relationship between them.
The earliest known physiological function of SHBG is to bind to sex hormones, thereby regulating their bioavailability48. The activity of hepatic lipase involved in HDL-C breakdown is stimulated by androgens, while high levels of SHBG can reduce free androgens, thus decreasing hepatic lipase activity and increasing HDL-C levels49. Furthermore, previous studies indicate that the interaction between AMP-activated protein kinase and peroxisome proliferator-activated receptor can regulate the expression of hepatic nuclear factor-4α, thereby upregulating SHBG expression. Moreover, hepatic nuclear factor-4α influences the transcription of numerous genes related to lipid metabolism, which may help explain the correlation between circulating SHBG levels and lipid metabolism50. In summary, while epidemiology has revealed an association between SHBG and blood lipids, the underlying biological mechanisms remain poorly understood. As for dyslipidemia being a significant risk factor for CHD and its involvement in the pathophysiology of atherosclerosis, these have already been confirmed by previous studies51,52. Low-density lipoprotein is considered the most important blood lipid component leading to atherosclerosis, which is consistent with our findings13. Currently, clinical trials have established statin as the cornerstone of lipid-lowering therapy for CHD53. Good adherence to lipid-lowering therapy and achievement of LDL-C control target can significantly reduce the occurrence of major adverse cardiovascular events in patients with CHD54. Of course, besides alterations in lipid levels, there are inevitably other mediators at play. Studies indicate that low SHBG is also associated with insulin resistance, obesity, and other manifestations of metabolic syndrome50, all of which contribute to the development of atherosclerosis55,56.
In current clinical practice, serum SHBG is generally considered to have significant diagnostic value in polycystic ovary syndrome, while in other situations, SHBG measurement is rarely performed57,58. The increased risk of dyslipidemia and CHD associated with low SHBG levels may be largely overlooked. Therefore, our findings can assist clinical investigators in reevaluating the significance and necessity of detecting this parameter. As for whether SHBG can serve as a crucial marker for assessing the occurrence of related diseases, further research is needed to explore this possibility. In addition, it is important to note that the phenotypes predicted by the genetic variations begins early in life, thereby providing an estimate of lifelong effects, which differs from traditional clinical studies that apply interventions or observe phenotypes only for a period of time20,59. This is particularly crucial for the causality revealed in this study, as it can be ascertained that the influence of lipid levels on CHD risk is a long-term cumulative effect20,59. Because MR reveals long-term effects, short-term interventions targeting SHBG and lipid levels may yield effects lower than the expected effect estimates obtained from this MR study60.
There is a significant gender disparity in the risk of CHD, with women having a much lower risk of new-onset coronary events and related all-cause mortality. However, this "gender protection effect" significantly diminishes following MI61. In fact, women have unique atypical risk factors that are associated with the prognosis of CVDs, such as pre-menopausal breast fat accumulation, which negatively affect cardiovascular function through the overexpression of sodium-glucose transporter 2 and inflammatory cytokines downregulating the breast sirtuins62,63. This suggests that the influence of gender on the pathogenesis of CVDs may be quite complex. Benefiting from the SHBG summary-level data stratified by gender, we attempted a sex-specific analysis. Unfortunately, due mainly to the "emerging" horizontal pleiotropy, we cannot conclude that there is a sex difference in the effect of SHBG on CHD risk. Considering the principle behind horizontal pleiotropy, it's possible that when conducting MR analysis using SHBG summary-level data from male and female samples separately, the effects of certain confounders be amplified or new confounders arise.
The main strength of our study is that we utilized large GWAS summary-level data to comprehensively investigate the interrelationships between SHBG, lipid profiles, and CHD. This is the first MR study to provide causal evidence that blood lipid levels mediated a considerable proportion of serum SHBG effect on CHD risk, and extensive sensitivity analyses were conducted to assess the robustness of the results. This study also has some limitations, and we have made extensive efforts to address them. First, the IVW method of bidirectional MR shows reverse causality between many phenotypes, but the effect size and/or significance levels are much smaller than those observed for forward causality. Furthermore, the Steiger directionality test validates the effectiveness of the vast majority of forward causality. Because the methodology of MR is inherently less susceptible to the spurious reverse causality, bidirectional MR can indeed suggest that two phenotypes drive each other, and this situation does not affect the validity of forward causality64. Second, there is mild horizontal pleiotropy in the MR analysis results for SHBG and HDL-C (p = 0.02), which could potentially violate assumption II and III, leading to inaccurate causal estimates40. Therefore, we did not establish the association between them. Third, there is sample overlap between SHBG and partial mediators. Nevertheless, one study suggests that 2-sample MR methods can be safely used for 1-sample MR when the sample size is large65. In addition, the minimal discrepancy observed in the results before and after MRlap correction could also suggests that sample overlap is unlikely to have a significant impact on the causal effect. Lastly, the difference in the mediation proportions calculated by the difference method and the product method is negligible, further indicating that the impact caused by sample overlap is minimal. Fourth, in the GWAS for CHD and MI, 23% of the participants are of non-European ancestry. Population stratification may introduce confounding of the relationship between genetic variants and outcome, thus posing a risk of violating assumption III66. However, we observed that the effect allele frequency of the GWAS sample population for these two outcomes and serum SHBG levels are essentially consistent. This suggests that the racial heterogeneity is minor, and it is unlikely to introduce perceptible bias. Fifth, to some extent, due to the large number of SNPs, almost all MR analyses exhibit considerable heterogeneity. Therefore, the IVW method uniformly employs random-effects model. Sixth, the GWAS involved in our MR study was conducted in European population, so our findings may be difficult to generalize to other ethnic groups.
Conclusion
High serum SHBG levels are causally associated with reduced risk of CHD, MI, and hypertension, in which the improvement of lipid profile largely mediates the causal effect of CHD risk reduction. Our study results further emphasize the close association between SHBG and lipid metabolism, which subsequently impacts the onset of CHD. However, due to some limitations, our findings still need to be further explored and confirmed by future studies.
Data availability
The summary-level data for high cholesterol and hypercholesterolemia is sourced from the Bristol University Data Repository (https://data.bris.ac.uk/data/dataset/pnoat8cxo0u52p6ynfaekeigi). For specific instructions on how to request and download the data, refer to the MRC IEU UK Biobank GWAS pipeline version 228. The summary-level data for SHBG can be obtained from the UK Biobank (https://www.ukbibank.ac.uk). The summary-level data for VLDL-C also originates from the UK Biobank resource (https://biobank.ndph.ox.ac.uk/showcase/label.cgi?id=220). The summary-level data for TC23, CHD29, and MI29 are sourced from publicly published GWAS. The summary-level data for TG, LDL-C, and HDL-C were obtained from the IEU OpenGWAS project (https://gwas.mrcieu.ac.uk/datasets). The summary-level data for hypertension, heart failure and atrial fibrillation & flutter originate from the FinnGen Consortium (https://finngen.gitbook.io/documentation/). Additionally, the summary-level data for SHBG, TC, LDL-C, and CHD can also be found in the GWAS Catalog (https://www.ebi.ac.uk/gwas/home). Datasets generated during the current study are included in the Supplementary Material, further inquiries can be directed to the corresponding authors.
References
Fortunati, N. Sex hormone-binding globulin: Not only a transport protein. What news is around the corner?. J. Endocrinol. Investig. 22, 223–234. https://doi.org/10.1007/bf03343547 (1999).
Simons, P., Valkenburg, O., Stehouwer, C. D. A. & Brouwers, M. Sex hormone-binding globulin: Biomarker and hepatokine?. Trends Endocrinol. Metab. 32, 544–553. https://doi.org/10.1016/j.tem.2021.05.002 (2021).
Ottarsdottir, K., Hellgren, M., Bock, D., Nilsson, A. G. & Daka, B. Longitudinal associations between sex hormone-binding globulin and insulin resistance. Endocr. Connect. 9, 418–425. https://doi.org/10.1530/ec-20-0141 (2020).
Ding, E. L. et al. Sex hormone-binding globulin and risk of type 2 diabetes in women and men. N. Engl. J. Med. 361, 1152–1163. https://doi.org/10.1056/NEJMoa0804381 (2009).
Cooper, L. A., Page, S. T., Amory, J. K., Anawalt, B. D. & Matsumoto, A. M. The association of obesity with sex hormone-binding globulin is stronger than the association with ageing—Implications for the interpretation of total testosterone measurements. Clin. Endocrinol. 83, 828–833. https://doi.org/10.1111/cen.12768 (2015).
Azene, Z. N. et al. Estrone, sex hormone binding globulin and lipid profiles in older women: An observational study. Climacteric 26, 114–120. https://doi.org/10.1080/13697137.2023.2165908 (2023).
Aribas, E., Kavousi, M., Laven, J. S. E., Ikram, M. A. & van Lennep, J. E. R. Aging, cardiovascular risk, and SHBG levels in men and women from the general population. J. Clin. Endocrinol. Metab. 106, 2890–2900. https://doi.org/10.1210/clinem/dgab470 (2021).
Canoy, D. et al. Serum sex hormone-binding globulin and testosterone in relation to cardiovascular disease risk factors in young men: A population-based study. Eur. J. Endocrinol. 170, 863–872. https://doi.org/10.1530/eje-13-1046 (2014).
Hammer, G. P., Prel, J. D. & Blettner, M. Avoiding bias in observational studies. Dtsch. Arztebl. Int. 106, 664–668. https://doi.org/10.3238/arztebl.2009.0664 (2009).
Li, J. et al. Sex hormone-binding globulin and risk of coronary heart disease in men and women. Clin. Chem. 69, 374–385. https://doi.org/10.1093/clinchem/hvac209 (2023).
Björkegren, J. L. M. & Lusis, A. J. Atherosclerosis: Recent developments. Cell 185, 1630–1645. https://doi.org/10.1016/j.cell.2022.04.004 (2022).
Sardu, C., Paolisso, G. & Marfella, R. Inflammatory related cardiovascular diseases: From molecular mechanisms to therapeutic targets. Curr. Pharm. Des. 26, 2565–2573. https://doi.org/10.2174/1381612826666200213123029 (2020).
Shaya, G. E., Leucker, T. M., Jones, S. R., Martin, S. S. & Toth, P. P. Coronary heart disease risk: Low-density lipoprotein and beyond. Trends Cardiovasc. Med. 32, 181–194. https://doi.org/10.1016/j.tcm.2021.04.002 (2022).
Sanderson, E. et al. Mendelian randomization. Nat. Rev. Method. Prim. 2, 21. https://doi.org/10.1038/s43586-021-00092-5 (2022).
Burgess, S. & Thompson, S. G. Mendelian Randomization: Methods for Causal Inference Using Genetic Variants 2nd edn, 19–20 (Chapman and Hall/CRC, 2021).
Emdin, C. A., Khera, A. V. & Kathiresan, S. Mendelian randomization. JAMA-J. Am. Med. Assoc. 318, 1925–1926. https://doi.org/10.1001/jama.2017.17219 (2017).
Hemani, G., Tilling, K. & Davey Smith, G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 13, e1007081. https://doi.org/10.1371/journal.pgen.1007081 (2017).
Sanderson, E. Multivariable Mendelian randomization and mediation. Cold Spring Harb. Perspect. Med. https://doi.org/10.1101/cshperspect.a038984 (2021).
Carter, A. R. et al. Mendelian randomisation for mediation analysis: Current methods and challenges for implementation. Eur. J. Epidemiol. 36, 465–478. https://doi.org/10.1007/s10654-021-00757-1 (2021).
Skrivankova, V. W. et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomisation (STROBE-MR): Explanation and elaboration. BMJ 375, n2233. https://doi.org/10.1136/bmj.n2233 (2021).
Skrivankova, V. W. et al. Strengthening the reporting of observational studies in epidemiology using Mendelian randomization: The STROBE-MR statement. JAMA 326, 1614–1621. https://doi.org/10.1001/jama.2021.18236 (2021).
Ruth, K. S. et al. Using human genetics to understand the disease impacts of testosterone in men and women. Nat. Med. 26, 252–258. https://doi.org/10.1038/s41591-020-0751-5 (2020).
Willer, C. J. et al. Discovery and refinement of loci associated with lipid levels. Nat. Genet. 45, 1274–1283. https://doi.org/10.1038/ng.2797 (2013).
Howe, L. J. et al. Within-sibship GWAS improve estimates of direct genetic effects. Genet. Epidemiol. 45, 801–801 (2021).
Davies, N. M. et al. Within family Mendelian randomization studies. Hum. Mol. Genet. 28, R170–R179. https://doi.org/10.1093/hmg/ddz204 (2019).
Klimentidis, Y. C. et al. Phenotypic and genetic characterization of lower LDL cholesterol and increased type 2 diabetes risk in the UK biobank. Diabetes 69, 2194–2205. https://doi.org/10.2337/db19-1134 (2020).
Julkunen, H. et al. Atlas of plasma NMR biomarkers for health and disease in 118,461 individuals from the UK Biobank. Nat. Commun. https://doi.org/10.1038/s41467-023-36231-7 (2023).
Ruth, M., Elsworth, B. L., Mitchell, R., Raistrick, C. A., Paternoster, L., Hemani, G., Gaunt, T. R. MRC IEU UK Biobank GWAS pipeline version 2. (2019). https://doi.org/10.5523/bris.pnoat8cxo0u52p6ynfaekeigi.
Nikpay, M. et al. A comprehensive 1000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat. Genet. 47, 1121. https://doi.org/10.1038/ng.3396 (2015).
Kurki, M. I. et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 613, 508–518. https://doi.org/10.1038/s41586-022-05473-8 (2023).
Burgess, S. & Thompson, S. G. Avoiding bias from weak instruments in Mendelian randomization studies. Int. J. Epidemiol. 40, 755–764. https://doi.org/10.1093/ije/dyr036 (2011).
Pierce, B. L., Ahsan, H. & Vanderweele, T. J. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int. J. Epidemiol. 40, 740–752. https://doi.org/10.1093/ije/dyq151 (2011).
Papadimitriou, N. et al. Physical activity and risks of breast and colorectal cancer: A Mendelian randomisation analysis. Nat. Commun. 11, 597. https://doi.org/10.1038/s41467-020-14389-8 (2020).
Bowden, J. et al. A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat. Med. 36, 1783–1802. https://doi.org/10.1002/sim.7221 (2017).
Burgess, S., Bowden, J., Fall, T., Ingelsson, E. & Thompson, S. G. Sensitivity analyses for robust causal inference from Mendelian randomization analyses with multiple genetic variants. Epidemiology 28, 30–42. https://doi.org/10.1097/ede.0000000000000559 (2017).
Lin, Z. T., Deng, Y. Q. & Pan, W. Combining the strengths of inverse-variance weighting and Egger regression in Mendelian randomization using a mixture of regressions model. PLoS Genet. 17, 25. https://doi.org/10.1371/journal.pgen.1009922 (2021).
Bowden, J., Smith, G. D., Haycock, P. C. & Burgess, S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40, 304–314. https://doi.org/10.1002/gepi.21965 (2016).
Burgess, S. & Thompson, S. G. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur. J. Epidemiol. 32, 377–389. https://doi.org/10.1007/s10654-017-0255-x (2017).
Bowden, J., Smith, G. D. & Burgess, S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 44, 512–525. https://doi.org/10.1093/ije/dyv080 (2015).
Verbanck, M., Chen, C. Y., Neale, B. & Do, R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 50, 693. https://doi.org/10.1038/s41588-018-0099-7 (2018).
Tofighi, D. & MacKinnon, D. P. RMediation: An R package for mediation analysis confidence intervals. Behav. Res. Methods 43, 692–700. https://doi.org/10.3758/s13428-011-0076-x (2011).
Burgess, S., Davies, N. M. & Thompson, S. G. Bias due to participant overlap in two-sample Mendelian randomization. Genet. Epidemiol. 40, 597–608. https://doi.org/10.1002/gepi.21998 (2016).
Mounier, N. & Kutalik, Z. Bias correction for inverse variance weighting Mendelian randomization. Genet. Epidemiol. 47, 314–331. https://doi.org/10.1002/gepi.22522 (2023).
Li, Y. X. et al. Causal effect of sex hormone-binding globulin and testosterone on coronary heart disease: A multivariable and network Mendelian randomization analysis. Int. J. Cardiol. 339, 179–184. https://doi.org/10.1016/j.ijcard.2021.06.037 (2021).
Haffner, S. M., Dunn, J. F. & Katz, M. S. Relationship of sex hormone-binding globulin to lipid, lipoprotein, glucose, and insulin concentrations in postmenopausal women. Metab.-Clin. Exp. 41, 278–284. https://doi.org/10.1016/0026-0495(92)90271-b (1992).
Pugeat, M. et al. Interrelations between sex hormone-binding globulin (SHBG), plasma-lipoproteins and cardiovascular risk. J. Steroid. Biochem. Mol. Biol. 53, 567–572. https://doi.org/10.1016/0960-0760(95)00102-6 (1995).
Gyllenborg, J. et al. Cardiovascular risk factors in men: The role of gonadal steroids and sex hormone-binding globulin. Metab.-Clin. Exp. 50, 882–888. https://doi.org/10.1053/meta.2001.24916 (2001).
Simó, R., Sáez-López, C., Barbosa-Desongles, A., Hernández, C. & Selva, D. M. Novel insights in SHBG regulation and clinical implications. Trends Endocrinol. Metab. 26, 376–383. https://doi.org/10.1016/j.tem.2015.05.001 (2015).
Bataille, V. et al. Sex hormone-binding globulin is a major determinant of the lipid profile: The PRIME study. Atherosclerosis 179, 369–373. https://doi.org/10.1016/j.atherosclerosis.2004.10.029 (2005).
Basualto-Alarcón, C. et al. Classic and novel sex hormone binding globulin effects on the cardiovascular system in men. Int. J. Endocrinol. 2021, 13. https://doi.org/10.1155/2021/5527973 (2021).
Malakar, A. K. et al. A review on coronary artery disease, its risk factors, and therapeutics. J. Cell. Physiol. 234, 16812–16823. https://doi.org/10.1002/jcp.28350 (2019).
Colantonio, L. D. et al. Association of serum lipids and coronary heart disease in contemporary observational studies. Circulation 133, 256–264. https://doi.org/10.1161/circulationaha.115.011646 (2016).
Goldstein, J. L. & Brown, M. S. A century of cholesterol and coronaries: From plaques to genes to statins. Cell 161, 161–172. https://doi.org/10.1016/j.cell.2015.01.036 (2015).
Mazhar, F. et al. Intensity of and adherence to lipid-lowering therapy as predictors of major adverse cardiovascular outcomes in patients with coronary heart disease. J. Am. Heart Assoc. 11, 34. https://doi.org/10.1161/jaha.122.025813 (2022).
Katta, N., Loethen, T., Lavie, C. J. & Alpert, M. A. Obesity and coronary heart disease: Epidemiology, pathology, and coronary artery imaging. Curr. Probl. Cardiol. 46, 26. https://doi.org/10.1016/j.cpcardiol.2020.100655 (2021).
Goodarzi, M. O. & Rotter, J. I. Genetics insights in the relationship between type 2 diabetes and coronary heart disease. Circ. Res. 126, 1526–1548. https://doi.org/10.1161/circresaha.119.316065 (2020).
Deswal, R., Yadav, A. & Dang, A. S. Sex hormone binding globulin—An important biomarker for predicting PCOS risk: A systematic review and meta-analysis. Syst. Biol. Reprod. Med. 64, 12–24. https://doi.org/10.1080/19396368.2017.1410591 (2018).
Zhu, J. L., Chen, Z., Feng, W. J., Long, S. L. & Mo, Z. C. Sex hormone-binding globulin and polycystic ovary syndrome. Clin. Chim. Acta 499, 142–148. https://doi.org/10.1016/j.cca.2019.09.010 (2019).
Holmes, M. V., Ala-Korpela, M. & Smith, G. D. Mendelian randomization in cardiometabolic disease: Challenges in evaluating causality. Nat. Rev. Cardiol. 14, 14. https://doi.org/10.1038/nrcardio.2017.78 (2017).
Swanson, S. A., Tiemeier, H., Ikram, M. A. & Hernán, M. A. Nature as a Trialist? Deconstructing the analogy between Mendelian randomization and randomized trials. Epidemiology 28, 653–659. https://doi.org/10.1097/ede.0000000000000699 (2017).
Sardu, C., Paolisso, G. & Marfella, R. Impact of sex differences in incident and recurrent coronary events and all-cause mortality. J. Am. Coll. Cardiol. 77, 829–830. https://doi.org/10.1016/j.jacc.2020.10.059 (2021).
Sardu, C. et al. Pre-menopausal breast fat density might predict MACE during 10 years of follow-up the BRECARD study. JACC-Cardiovasc. Imag. 14, 426–438. https://doi.org/10.1016/j.jcmg.2020.08.028 (2021).
Sardu, C. et al. SGLT2 breast expression could affect the cardiovascular performance in pre-menopausal women with fatty vs. non fatty breast via over-inflammation and sirtuins’ down regulation. Eur. J. Intern. Med. 113, 57–68. https://doi.org/10.1016/j.ejim.2023.04.012 (2023).
Deng, M. G. et al. Association between frailty and depression: A bidirectional Mendelian randomization study. Sci. Adv. 9, eadi3902. https://doi.org/10.1126/sciadv.adi3902 (2023).
Minelli, C. et al. The use of two-sample methods for Mendelian randomization analyses on single large datasets. Int. J. Epidemiol. 50, 1651–1659. https://doi.org/10.1093/ije/dyab084 (2021).
Sanderson, E., Richardson, T. G., Hemani, G. & Davey Smith, G. The use of negative control outcomes in Mendelian randomization to detect potential population stratification. Int. J. Epidemiol. 50, 1350–1361. https://doi.org/10.1093/ije/dyaa288 (2021).
Acknowledgements
The authors offer their thanks and appreciation to all the investigators and consortiums for making the summary-level data used in this study.
Funding
This work was supported by grants from the Zhejiang Traditional Chinese Medicine Science and Technology Program (2023ZL184).
Author information
Authors and Affiliations
Contributions
J.T.Y., J.D.Z. and W.L.T. designed the study, and contributed to the data collection and data analysis. Data reduction and graphics making were performed by all authors. J.T.Y. drafted the manuscript. W.L.T. performed the final approval of the version to be published. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, J., Zhou, J., Liu, H. et al. Blood lipid levels mediating the effects of sex hormone-binding globulin on coronary heart disease: Mendelian randomization and mediation analysis. Sci Rep 14, 11993 (2024). https://doi.org/10.1038/s41598-024-62695-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62695-8
Keywords
This article is cited by
-
Association of ultra-processed food-related metabolites with selected biochemical markers in the UK Biobank
Nutrition Journal (2025)
-
Causal relationship between immune cells and osteoporosis based on genetic prediction: a bidirectional two-sample mediated Mendelian randomization analysis
Scientific Reports (2025)