Abstract
Emerging evidence underscores the role of metabolites in immunomodulation. We surmise that specific metabolic signatures might be conserved during repeated Omicron infections. To verify our hypothesis, patients with first (n = 28) and repeated Omicron infections (n = 38) between November 2023 to April 2024 were recruited into this study. Healthy controls (n = 20) were enrolled in the same period. Comprehensive serum metabolome and lipidome were quantitated using mass spectrometric approaches. The neutralizing activity of sera against the pseudotyped Omicron variant JN.1 was determined. Circulating cytokines/chemokines were quantified using a Bioplex Kit Assay. The proportion of severe/moderate infections was 2.9-fold higher in first infection patients compared to reinfection patients (67.9% vs. 23.7%, p = 0.004). Geometric mean titers (GMT) for the Omicron variant JN.1 were higher in moderate/severe infections than mild infections, but non-significant between first and repeated infections. We observed perturbed coregulation between plasma indoles and circulating plasmalogen phospholipids in Omicron-infected patients, while disrupted histidine-triacylglycerol coregulation was specific to first-infections. A panel of three lasso-selected metabolites (SL d18:1/22:0 h, tetra-peptide Pro Tyr Tyr Val, and 1,2,3,4-Tetrahydroisoquinoline) effectively differentiated moderate/severe Omicron infections from mild ones (AUROC at 0.917, 95% CI 0.793-1.000). Our findings highlight modifiable metabolic signatures as possibly new therapeutic interventions against rapidly evolving variants of SARS-CoV-2.
Similar content being viewed by others
Introduction
Since December 2019, coronavirus disease (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has posed a formidable threat to public health worldwide1. By far, the SARS-CoV-2 virus has undergone rapid evolution and diversified into many lineages including D614G, Beta/Gamma, Delta, and more recently, the Omicron1. Of these lineages, the Omicron variant is the most heavily mutated, with more than 30 mutated sites in the Spike protein, resulting in enhanced transmissibility ascribed to increased binding capacity to the human angiotensin converting enzyme 2 (hACE2) receptor2. Aligned with findings based on genomic sequences, the rate of Omicron infection is remarkably high, which triggered another global wave of the SARS-CoV-2 outbreaks following its first emergence in November 20213. Despite the lower percentages of severe infections for Omicron variants compared to previous lineages, approximately 0.08–29.1% of infected patients died from Omicron infection and/or its complications5. As a result, Omicron was designated as a variant of concern (VOC) by the Centers for Disease Control and Prevention.
While vaccination remains a powerful tool to boost immune protection, neutralizing antibodies (Nabs) in the sera of vaccinated individuals determined using pseudovirus assay revealed considerably lower Nabs toward Omicron relative to wild type virus6,7. Indeed, immune imprinting, which limits vaccine efficacy for prevention of infection, was reportedly higher for the Omicron variant, attributed to its distinctive serotype from wild-type SARS-CoV-28. Physically, an individual who has recovered from past SARS-CoV-2 infection possesses acquired immunity against the infectious lineage for a certain duration. Results from a meta-analysis involving 65 studies from 19 countries showed that protection bestowed by past infection against re-infection from ancestral, alpha, and delta variants remained high at 78.6% for up to 40 weeks. In sharp contrast, acquired immunity against Omicron BA.1 declined to 36.1% (95%CI, 24.4-51.3%) by week 409. Put together, these data suggest that vaccination and innate immunity against Omicron is not sufficiently strong to prevent reinfection. Exploration of therapeutic targets to gain better protection from Omicron reinfection is urgently required to mitigate disease burden.
Intracellular metabolites are crucial regulators of cellular immune function10. For instance, upon stress, increased levels of acetate expand the acetyl-CoA pool and promotes GAPDH acetylation, both of which drive glycolysis and promote memory CD8+ T cell response for pathogen clearance11. Manipulating host metabolism may offer new strategy to increase antivirulence and downscale inflammatory response during infections. With particular relevance to Omicron infections, the rapid rate of viral mutations may hinder the development of an effective and durable vaccination. While the virus may rapidly evolve, the triggered metabolic pathologies are “old” and generalizable, which eventually converge on common dysregulated pathways that lead to the demise of the host12. Therefore, targeting host metabolism represents a viable option to upscale defense against continual waves of SARS-CoV-2 outbreaks, particularly in terms of tackling variants like Omicron with high mutation rate. Despite preceding metabolomics studies have explored metabolic features of Omicron-infected patients13,14comprehensive characterization of conserved metabolic features and their biological implications in patients with repeated Omicron infections is lacking by far.
We postulate that specific metabolic pathologies are conserved across multiple instances of Omicron infections that may denote new therapeutic targets for intervention. Herein, we screened for circulating metabolites associated with disease severity that were reproduced amongst first infection and reinfection patients, and explored the implicated metabolic pathways through integration of metabolomics and lipidomics data with clinical phenomes comprising biochemical features and measures of immune responses.
Results
Study design and participant demographics
Figure 1A shows the study design. Table 1 lists the general characteristics of the study participants. Participants ranged in age from 18 to 85 years, with the mean (SD) ages summarized in Table 1. Compared with healthy controls, patients with first infection and reinfection of Omicron had lower LDL-c (P < 0.05) and fasting plasma glucose (P = 0.052 for first infection, P = 0.040 for reinfection), while HDL-c was marginally decreased only in reinfection patients (P = 0.064). Reinfection patients also exhibited significantly reduced serum triglycerides compared to healthy controls (P = 0.040). The proportion of moderate/severe infections was 2.9-fold higher in first infection patients than reinfection patients (67.9% vs. 23.7%, P = 0.004).
Study design and clinical demographics. (A) This study enrolled a group of healthy controls (n = 20), patients first infected with Omicron (n = 28) and patients repeatedly infected with Omicron (n = 38) during the Omicron outbreak from November 2023 to April 2024. High-coverage, quantitative targeted lipidomics and untargeted metabolomics were conducted on fasting plasma samples collected within 7 days of symptom onset to elucidate metabolic features associated with Omicron infections. (B,C) Changes in the levels of neutralizing antibodies (Nabs) against Omicron JN.1 (B) and selected plasma cytokines including IL-1RA, IP-10, IL-7 and MDC. (C) across healthy controls (n = 20), first infection (n = 28) and reinfection (n = 38) Omicron patients categorized by different disease severity (mild and moderate/severe). In all boxplots, median is indicated by the horizontal line and the first and third quartiles are represented by the box edges. The lower and upper whiskers extend from the hinges to the smallest and largest values, respectively, with individual samples indicated as dots. P values of pairwise comparisons based on two-sided Games-Howell test were presented using letter-based representation, with two groups sharing a common letter being not statistically different at P < 0.05.
Neutralizing antibody titers against JN.1
Using pseudovirus neutralization assay, the geometric mean titers (GMT) for Omicron variant JN.1 were 2.2 for reinfection patients, which was decreased by 30.0% and 11.3% when compared with healthy controls and first infection patients, respectively (P < 0.05for both) (Fig. 1B, left). When patients were categorized by severity, GMTs against JN.1 were significantly higher in moderate/severe infections compared to mild ones for both first infection and reinfection patients (Fig. 1B, right).
Changes in cytokine and chemokine profiles
In parallel to Nab quantification, Table 2 outlines changes in circulating cytokines and chemokines in first infection and reinfection patients compared to healthy controls. Plasma levels of sCD40L, EGF, GRO-α, IL-7, PDGF-AA, PGDF-AB/BB and VEFG-A were consistently reduced in both first infection and reinfection compared to healthy controls, while IL-1RA, IL-10, IL-18, IP-10, MCP-1 and M-CSF were increased. In addition, IL-14 and MDC were elevated and reduced, respectively, only in first infection patients compared to healthy controls. Specific cytokines exhibited significant changes across differing severity of infections (Fig. 1C). IL-1RA, IP-10 were marginally reduced in moderate/severe infections relative to mild infections, while IL-7 was elevated. On the other hand, MDC was specifically low in moderate/severe cases of first infection.
Conserved plasma metabolome signatures between first infection and reinfection
In all, a repertoire of 518 metabolites from 90 subcategories were quantitated. Top differential metabolites in infected patients relative to healthy controls, such as alanylaspartic acid and lactic acid, were conserved between first infection and reinfection as illustrated in volcano plots (Fig. 2A). Venn diagram indicates a total of 95 differential metabolites that overlapped between first infection and reinfection (Fig. 2B), and circus plot outlines top 30 overlapping differential metabolites between first infection and reinfection relative to healthy controls based on ascending P values (Fig. 2C). ORA of overlapping differential metabolites against the human small molecule pathway database (hSMPD) revealed glutathione metabolism, nicotinate and nicotinamide metabolism, and Warburg effect as top aberrant metabolic pathways conserved between first infection and reinfection (Fig. 2D).
Plasma metabolome signatures of Omicron infections. For all pairwise comparisons, P values from two-sided Student’s t-test were presented, where n = 20 for healthy controls, n = 28 for first infection and n = 38 for reinfection Omicron patients. (A) Volcano plots illustrate differential plasma metabolites in first infection (left panel) and reinfection (right panel) patients compared to healthy controls. (B) Venn diagram displays the number of significant (P < 0.05) differential metabolites that overlapped between first infection compared to healthy controls and reinfection compared to healthy controls. (C) Circos plot illustrates top 30 differential metabolites ranked by ascending P values in first infection patients (inner rim) and reinfection patients (outer rim) relative to healthy controls. * P < 0.05, ** P < 0.01, *** P < 0.001. Color bar indicates log2(fold-change), where red indicates increase and blue indicates decrease in moderate/severe infection relative to mild infection, respectively. (D) Over-representation analysis of dysregulated pathways from the small molecule pathway database (SMPD) based on differential metabolites that were conserved between first infection and reinfection patients compared to healthy controls. (E) Venn diagram displays the number of significant (P < 0.05) metabolites in moderate/severe infections compared to mild infections that were conserved between first infection and reinfection Omicron patients. (F) Barplot on the percentages of differential metabolites (P < 0.05) in moderate/severe infections relative to mild infections that were conserved between first infection and reinfection patients. (G) Circos plot illustrates top 30 differential metabolites ranked by ascending P values in moderate/severe infections relative to mild infections amongst first infection patients (inner rim) and reinfection patients (outer rim). * P < 0.05, ** P < 0.01, *** P < 0.001. Color bar indicates log2(fold-change), where red indicates increase and blue indicates decrease in moderate/severe infection relative to mild infection, respectively. (H) Over-representation analysis of dysregulated pathways from the small molecule pathway database (SMPD) based on differential metabolites between moderate/severe infections compared to mild infections that were conserved in first infection and reinfection patients. FC, fold change; LysoPE, lysophosphatidylethanolamine; LysoPC, lysophosphatidylcholine.
We next compared differential metabolites between moderate/severe infections relative to mild infections, respectively, which uncovered 107 differential metabolites that were conserved between first infection and reinfection patients (Fig. 2E). It is noteworthy that first infection patients exhibited a lower percentage of conserved differential metabolites associated with phenotype severity (or a higher percentage of unique differential metabolites) (Fig. 2F), suggesting distinct metabolic regulation of innate immunity against the Omicron virus specific to first infection. Notably, reductions in several sn-1 LysoPCs were observed in moderate/severe infections compared to mild infections in both first infection and reinfection patients (Fig. 2G). ORA of overlapping differential metabolites underscores gluconeogenesis as the top aberrant pathway conserved between both first infection and reinfection, which was significantly upregulated in moderate/severe patients compared to mild patients (Fig. 2H).
Conserved plasma lipidome signatures between first infection and reinfection
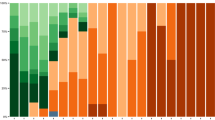
A library of 565 lipids from 27 classes was quantitated in the plasma of the study participants (Fig. 3A). Volcano plots of first infection and reinfection patients compared to healthy controls revealed general increases in plasma acylcarnitines and reductions in phosphatidylserines (PS) (Fig. 3B-C). When comparing moderate/severe infections relative to mild infections, consistent reductions in PE-Os were observed for both first infection and reinfection patients (Fig. 3D-E). Plasma levels of various sphingomyelins (SMs), sulfatides (SLs), PE-Os, ceramides (Cer), ceramide-1-phosphates (Cer1P), lysophosphatidic acids (LPAs) and lysophosphatidylcholines (LPCs) were consistently reduced in both first infection and reinfection cases compared to healthy controls, while free fatty acids (FFAs) were elevated (Fig. 3F). As we systematically compared overlapping differential lipids between first infection and reinfection, and which displayed progressive changes in patients relative to healthy controls, as well as moderate/severe infections relative to mild infections, only summed PE-O was conserved across all comparisons (Fig. 3F). The summed levels of PE-Os exhibited progressive reductions from healthy controls to mild infection to moderate/severe infections, and were consistently significantly different across both first infection and reinfection patients (Fig. 3G). Numerous other plasma PE-Os also displayed progressive decreases in Omicron-infected patients (Fig. 3H), and hierarchical clustering based on individual PE-O species further confirmed this trend, with distinct clustering patterns observed across healthy controls, first infection, and reinfection subgroups (Fig. 3I).
Plasma lipidome signatures of Omicron infections. For all pairwise comparisons, P values from a two-sided Student’s t-test were used (n = 20 healthy controls, n = 28 first infection, n = 38 reinfection Omicron patients). (A) Radar plot of plasma lipidome diversity comprising 565 lipids from 27 classes. (B-E) Volcano plots illustrate differential plasma lipids in first infection (B) and reinfection (C) patients versus healthy controls, as well as in moderate/severe infections relative to mild infections amongst first infection (D) and reinfection (E) patients, respectively. (F) Circos plot ranks the top 30 differential lipids in moderate/severe infections (inner rim: first infection, outer rim: reinfection). * P < 0.05, ** P < 0.01, *** P < 0.001. Color bar indicates log2(fold-change): red (increase), blue (decrease) in severe vs. mild cases. (G) Venn diagrams display the number of significant (P < 0.05) lipids that were conserved between Omicron infection (infected vs. healthy controls) and symptom severity (moderate/severe vs. mild infections) in both first infection and reinfection patients. (H) Boxplot illustrates changes in summed PE-Os across healthy controls (n = 20), first infection mild patients (n = 9), first infection moderate/severe patients (n = 19), reinfection mild patients (n = 27), reinfection moderate/severe patients (n = 11). Median is indicated by the horizontal line and the first and third quartiles are represented by the box edges. The lower and upper whiskers extend from the hinges to the smallest and largest values, respectively, with individual samples indicated as dots. P values of pairwise comparisons based on two-sided Games-Howell test were presented using letter-based representation, with two groups sharing a common letter being not statistically different at P < 0.05. (I) Heatmap displays changes in individual PE-O species across healthy controls (n = 20), first-infection mild patients (n = 9), first infection moderate/severe patients (n = 19), reinfection mild patients (n = 27), reinfection moderate/severe patients (n = 11). Lipid levels were expressed and plotted as Z-scores. BMP, bis(monoacylglycerol)phosphate; CE, Cholesterol ester; Cer, ceramides; Cer1P, ceramide-1-phosphate; DAG, diacylglycerol; FFA, free fatty acid; Gb3, globotroaosylceramide; GluCer, glucosylceramide; LacCer, lactosylceramide; LPA, lysophosphatidic acid; LPC, lysophosphatidylcholine; LPE, lysophosphatidylethanolamine; LPI, lysophosphatidylinositol; PA, phosphatidic acid; PC, phosphatidylcholine; PC-O, plasmalogen phosphatidylcholine; PE, phosphatidylethanolamine; PE-O, phosphatidylethanolamine; PG, phosphatidylglycerol; PI, phosphatidylinositol; PS, phosphatidylserine; SIP, sphingosine-1-phosphate; SL, sulfatide; SM, sphingomyelin; Sph, sphingosine; TAG, triacylglycerol.
Differential lipid-metabolite coregulation in Omicron infection
Endogenous abundances of coregulated metabolites along a common pathway are often correlated, and therefore changing metabolite correlations across different biological conditions are indicative of perturbed metabolic coregulation15,16. We leveraged differential correlation analyses for integration of lipidome and metabolome data to decipher pathologically relevant metabolic dysregulation in patients with Omicron infections17. Lipid-metabolite correlations were calculated using the R package DGCA, and MEGENA was leveraged to construct networks from differentially correlated lipid-metabolite pairs in first infection patients relative to healthy controls (Fig. 4A), and repeated infection patients relative to healthy controls (Supplemental Fig. 1), respectively.
Trans-omics integration of lipidome and metabolome changes. (A) MEGENA network illustrates differential correlations between lipid and metabolites in first infection (n = 28) relative to healthy controls (n = 20). Only lipid/metabolite pairs with significant differential correlations (pValDiff < 0.0001) were included. Sign/sign indicates direction and strength of correlation in healthy controls and first infection, respectively, and number that follows indicates number of lipid/metabolite pairs in the global network exhibiting this pattern of change. For instance, mustard yellow edges +/0 (357) in the upper legend of the global network indicates that correlation between connected lipid/metabolite pair was positive + in healthy controls, and the correlation was lost (became 0) in first infection patients. Two modules of interest were boxed and enlarged for emphasis. (B) Over-representation analysis of dysregulated pathways from the Kyoto Encyclopedia of Genes and Genomes (KEGG) database based on differential metabolites (P < 0.05 from Student’s t-test) between first infection patients (n = 28) relative to healthy controls (n = 20). (C) Boxplots of changes in specific metabolites and lipids from Module I (upper panel) and Module II (lower panel) of the global differential correlation network. In all box plots, the median is indicated by the horizontal line and the first and third quartiles are represented by the box edges. The lower and upper whiskers extend from the hinges to the smallest and largest values, respectively, with individual samples indicated as dots. P values from Student’s t-test were indicated using a letter-based representation with two groups sharing a common letter being not statistically different at P < 0.05. TCA, tricarboxylic acid; PE-O, plasmalogen phosphatidylethanolamine; TAG, triacylglycerol.
We noticed a central module comprising indole connected to numerous PE-Os and plasmalogen PCs (PC-Os) via red (+/-) and yellow (+/0) edges (Fig. 4A, module I), reflecting positive correlations in healthy controls that became negative or were lost in first infection patients. A similar module connecting indole and plasmalogen phospholipids was observed in the global network of differential correlations for patients with repeated infections compared to healthy controls (Supplementary Fig. 1). These results indicate consistently perturbed coregulation between plasma levels of indoles and plasmalogen phospholipids in patients with first or multiple instances of Omicron infections.
A module with L-histidine as a central hub connected to several triacylglycerol (TAG) species with yellow (+/0) edges was specifically observed in patients with first Omicron infection relative to healthy controls (Fig. 4A, module II). It is noteworthy that both indole and histidine are closely implicated in gut microbial metabolism. Indole is produced from the essential amino acid L-tryptophan by gut microbiome, while decarboxylation of L-histidine by gut microbes generates histamine18. Accordingly, over-representation analysis (ORA) of metabolic pathways from the KEGG database based on metabolites uniquely altered in patients with first Omicron infection showed that “histidine metabolism” and “tryptophan metabolism” were amongst the top dysregulated pathways (Fig. 4B).
Plasma levels of indole and precursor L-tryptophan were significantly reduced in patients with Omicron infections relative to healthy controls, and similar trend was observed for plasma PE-Os (Fig. 4C, upper panel). On the other hand, L-histidine was reduced in patients, with concurrent increase in plasma TAGs only in patients with first Omicron infection (Fig. 4C, lower panel).
In patients infected with Omicron, plasma indole levels were negatively correlated with lymphocyte count, while PE-Os were positively correlated (Fig. 5A). In patients first infected with Omicron, circulating L-histidine was positively correlated with alanine transaminase (ALT) activity and negatively correlated with IL1-RA; while plasma TAGs were expectably and positively correlated with serum triglycerides and LDL-C and negatively correlated with numerous inflammatory cytokines, particularly IFN-γ and IL-6 15–18(Fig. 5B).
Correlations with clinical demographics and laboratory biochemistry. Correlation plots illustrate spearman correlations between clinical indices and specific plasma metabolites and lipids in Module I and Module II of the MEGENA global network. Only correlations with P < 0.05 were indicated with colored circles. Positive correlations were shown in red and negative correlations were shown in blue, with sizes of circles representing the strength of the significance p-value and intensity of color representing the magnitude of the correlation coefficients. (A) Correlation analyses between plasma indoles and PE-Os with clinical and biochemical measures amongst Omicron-infected patients (n = 66). (B) Correlation analyses between plasma L-histidine and top 30 differential TAGs with clinical and biochemical measures amongst first infection Omicron patients (n = 28). Differential TAGs were selected based on ascending P values from Student’s t-test between first infection patients (n = 28) and healthy controls (n = 20). PE O, plasmalogen phosphatidylethanolamine; CRP, C-reactive protein; ALT, alanine transaminase; HDL-c, high-density lipoprotein cholesterol; LDL-c, low-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate; sCD40L, soluble cluster of differentiation 40 ligand; EGF, epidermal growth factor; FGF-2, fibroblast growth factor 2; FLT-3 L, FMS-like tyrosine kinase 3 ligand; G-CSF, granulocyte colony stimulating factor; GM-CSF, granulocyte-macrophage colony stimulating factor; GRO-alpha, growth regulated protein alpha; IFN, interferon; IL, interleukin; MCP, monocyte chemoattractant protein; MDC, macrophage-derived chemokine; MIG, monokine induced by interferon-gamma; MIP, macrophage inflammatory protein; PDGF, platelet-derived growth factor; RANTES, regulated upon activation, normal T cell expressed and presumable secreted; TGF, transforming growth factor; TNF, tumor necrosis factor; VEGF, vascular endothelial growth factor; TAG, triacylglycerol; CRP, C-reactive protein. ALT, alanine transaminase.
Metabolite panel differentiating moderate/severe infection from mild infection
Next, we performed lasso analysis on the common lipids and polar metabolites significantly altered in moderate/severe infections relative to mild infections (Figs. 2E and 3F), and three metabolites (variables) including SL d18:1/22:0 h, the tetra-peptide Pro Tyr Tyr Val, and 1,2,3,4-Tetrahydroisoquinoline were selected for subsequent logistic regression modeling based on optimal λ (Fig. 6A). Plasma levels of SL d18:1/22:0 h and Pro Tyr Try Val were inversely associated with severity of Omicron infection, while 1,2,3,4-Tetrahydroisoquinoline was positively associated (Fig. 6B). Incorporating age and gender as covariates, we randomly split the group of Omicron-infected patients into train set (70%) and test set (30%), the model obtained was able to differentiate moderate/severe infections from mild infections with a satisfactory area under receiver operating characteristic curve (AUROC) at 0.917 (95% CI 0.793-1.000) (Fig. 6C).
Metabolite panel segregating Omicron-infected patients of different severity. (A) Plot of test MSE by log (λ) value from lasso analysis that selects significant variables differentiating moderate/severe infections from mild infections amongst Omicron-infected patients (n = 66) based on optimal λ. (B) Three lasso-selected variables that discriminate Omicron-infected patients of different disease severity. (C) Area under receiver operating characteristic curve illustrates the performance of three lasso-selected variables in differentiating Omicron patients of different severity, with age and gender as covariates. AUC, area under the curve; Log, logarithm; ROC, receiver operating curve; FC, fold change; SL, sulfatide; Pro, proline; Tyr, tyrosine; Val, valine.
Discussion
We conducted the first comprehensive study dissecting systemic differences in metabolome and lipidome signatures between first and repeated Omicron infections. We observed higher percentage of moderate/severe infections in cases of first Omicron infection compared to reinfection. Our findings also illuminate aberrant glucose and nicotinamide metabolism as common metabolic disturbances conserved between first infection and reinfection by the Omicron virus. Many viruses such as SARS-CoV-2 are known to induce glycolysis in host cells to take advantage of the glycolytic environment for their replications19. The Warburg effect essentially entails preferential utilization of aerobic glycolysis over oxidative phosphorylation for ATP production, resulting in high lactate production in spite of adequate oxygen concentration. Although the yield of ATPs per molecule of glucose is lower for aerobic glycolysis, the rate of energy production is 10-1000 times faster20. Enveloped viruses like SARS-CoV-2 depend entirely on host cells to provide energy and raw materials for virion assembly. Induction of a Warburg-like state therefore allows rapid energy provision to meet the high energy demand of nucleic acid replication and virion packaging to facilitate viral transmission. Furthermore, modification of carbon source utilization may increase biomass availability for virion packaging6. Suppressing lactate overproduction may represent a plausible metabolic strategy to curb intercellular transmission of the Omicron virus. Consistent with preceding observations that coronavirus infection depletes cellular nicotinamide adenine dinucleotide (NAD+) levels21we observed downregulation of nicotinate and nicotinamide metabolism in Omicron-infected patients. Nutritional supplementation to boost NAD levels may be metabolically beneficial in terms of enhancing innate immunity against coronaviruses, mediated by Poly(ADP-ribose) polymerase (PARP) activity that is associated with cellular antiviral response21.
Apart from host metabolism alone, emerging evidence suggests a symbiotic coregulation between gut microbiota and the host immune system in response to viral infections. Physiologic concentrations of indole and its derivatives were shown to inhibit the chlorinating activity of myeloperoxidase (MPO) in neutrophils, which serve as a first line of defense against invading pathogens22. Notably, the vinyl ether linkages of plasmalogen phospholipids are specifically targeted by reactive chlorinating species produced by MPO23,24. Tryptophan-derived indoles alleviate inflammation-triggered bystander tissue damages and protect plasmalogen phospholipids from oxidative degradation against chlorinating activity of neutrophils25. Disrupted indole production may therefore account for diminished levels of circulating indoles in Omicron-infected patients. Aligned with this postulation, numerous Bifidobacteria that are major indole producers26 were reportedly lowered in the fecal samples of patients infected with SARS-COV-227. The significant correlations with circulating lymphocyte count also indicates that metabolic crosstalk between indoles and PE-Os might partake in the establishment of adaptive immunity in Omicron-infected patients. Mechanistically, PE-Os are well-known substrates of oxidative degradation, particularly under neutrophil-mediated oxidative stress. Myeloperoxidase (MPO), abundantly released from activated neutrophils during viral infections, catalyzes the production of hypochlorous acid, which selectively targets the vinyl-ether bond in PE-Os, resulting in their depletion23,24. Consistent with this, Omicron infections were associated with elevated inflammatory cytokines and neutrophil activation markers in our cohort, which may contribute to enhanced oxidative degradation of PE-Os. Additionally, given that plasmalogens play critical roles in modulating membrane fluidity and protecting against lipid peroxidation, the decrease of PE-Os may exacerbate membrane vulnerability, thereby aggravating host cell damage during Omicron infection. This hypothesis is supported by similar findings in severe COVID-19 patients in previous studies28,29. Further studies to directly link MPO activity and PE-O degradation in Omicron infection are warranted.
In contrast to indole that is a microbial metabolic product, histidine serves as a key energy substrate for gut microbiota. Decarboxylation of histidine by host or microbial enzymes yields histamine30which promotes IL-1 production that initiates cytokine storm and inflammatory cascade in COVID-1931. Measurement of histamine in plasma samples, however, is challenging due to its short half-life (~ 10–30 min)32. Preceding report underscores a strong inverse association between circulating histidine and liver steatosis. Circulating histidine was negatively associated with Proteobacteria but positively associated with healthy gut microbiota, such as Faecalibacterium and Bifidobacterium that do not possess histidine utilization system33. In addition, mice receiving fecal microbiota transplantation from human donors with high plasma histidine developed higher quantities of Bifidobacterium with dose-dependent reductions in hepatic expressions of genes implicated in de novo biosynthesis of fatty acids and cholesterol33. Reductions in plasma L-histidine and elevated circulating TAGs observed in first infection patients were therefore aligned with a plausible shift in gut microbiota toward histidine utilizers, which were associated with higher hepatic lipogenesis. Indeed, we observed significant coregulation between reduction in plasma histidine and liver function measured in terms of ALT. A previous study evaluating gut microbiome composition in COVID-19 patients revealed depletion of Faecalibacterium and Bifidobacterium in infected patients up to 30 days after disease resolution27. The molecular rationale for increases in circulating TAGs specifically in first Omicron infection warrants further investigation, but TAG-rich lipoproteins represent components comprising the innate, non-adaptive host immune response to infection. Corroborating our observations, L-histidine was negatively correlated with levels of the anti-inflammatory cytokine IL-1RA, a member of the IL-1 family predominantly involved in innate immunity. IL-1RA is readily secreted and is an antagonist of the IL-1 receptor, which serves to suppress proinflammatory innate responses triggered by other IL-1 cytokines34. Infection-triggered hyperlipoproteinemia scavenges pathogens in the circulation that are subsequently cleared by the liver, thus dampening the acute-phase response and ameliorating further cytokine stimulation35aligned with the negative correlations between circulating TAGs and inflammatory cytokines observed in first infection patients.
A panel of three lasso-selected metabolites (SL d18:1/22:0 h, tetrapeptide PYYV and 1,2,3,4-Tetrahydroisoquinoline) was demonstrated to effectively segregate moderate/severe infections from mild infections. Diminished plasma levels of hydroxylated SL d18:1/22:0 h and PYYV were associated with more severe clinical manifestations of Omicron infections. Many food-derived peptides have reported roles in modulating gut homeostasis and function36. For example, dietary supplementation of the dipeptide VY was demonstrated to reverse high-fat diet-induced gut dysbacteriosis by increasing the abundances of beneficial gut microbes including Faecalibacterium and Bifidobacterium. Plasma levels of several hydroxylated SLs were consistently lowered in moderate/severe infections compared to mild infections amongst both first infection and reinfection patients. Circulating hydroxylated SLs are implicated in hepatic immunomodulation via crosstalk with specific immune cell populations. On another note, increases in tetrahydroisoquinolines with severity of infections may be ascribed to antibiotic usage in Omicron-infected patients37. Our observations on consistent reductions in several sn-1 LysoPCs with severity of infection in both first infection and reinfection patients were aligned with the known role of secreted phospholipase A2 (PLA2) in the pathobiology of SARS-CoV-2 infection and its associated mortality rate29. PLA2 cleaves fatty acyls esterified to phosphatidylcholines (PCs), the major lipid constituents of cellular membranes, at the sn-2 positions to generate sn-1 LysoPCs while releasing FFAs. Reductions in plasma sn-1 LysoPCs hence suggest attenuated PLA2 activity in moderate/severe infections. Along this line, FFA binding pocket at the receptor binding ___domain of the Spike protein was shown to be conserved across pathogenic strains of β-coronaviruses infecting humans. FFA binding by linoleic acid stabilizes the locked confirmation, which is incompatible with ACE2 receptor binding, thereby impeding viral infection and transmission. FFA binding also triggers locked confirmation, which hinders with virion packaging within infected cells38. Antivirals targeting PLA2 activity modulate FFA release, thereby providing a plausible metabolic strategy to ameliorate severe symptom manifestations in Omicron infections. Altered levels of unsaturated fatty acids such as FA 22:4, FA 22:5 and FA 18:1 observed in Omicron-infected patients may be partially influenced by dietary factors. FA 22:5 and FA 22:4 are long-chain polyunsaturated fatty acids (PUFAs) that can be derived from dietary sources such as fish oil and meat, or endogenously synthesized from essential fatty acids via elongation and desaturation pathways. FA 18:1 (oleic acid) is abundant in olive oil and other plant-based oils. Changes in these fatty acids may not only reflect dietary intake, but also systemic inflammatory status, hepatic lipid remodeling, or mobilization of energy substrates under infection stress. Future studies integrating dietary intake records with lipidomics data will be needed to further dissect the diet-inflammation-lipidome axis in COVID-19 patients. While this study focused on infection status and disease severity, future investigations with larger cohorts are warranted to systematically evaluate sex-specific differences in the metabolic and lipidomic responses to Omicron infection.
Materials and methods
Study participants
This study complied with the Declarations of Helsinki for conducting investigations based on human participants, and was approved by the Institutional Review Board of the Beijing Youan Hospital (#2024-093). All participants were from the Chinese Han population and provided written informed consent. The enrollment period was from November 2023 to April 2024. The criteria of first Omicron infection were that the patients were not infected by Omicron before November 2023 and infected only once in the recruitment period. COVID-19 reinfection was defined as a SARS-CoV-2 positive test at least 90 days after the initial positive test; this time frame of 90 day was specified to reduce the probability that a positive test was related to the first infection. For healthy subjects, they were not infected with Omicron during the recruitment period.
Biochemical measurements
Fasting venous blood samples were collected into EDTA-containing anticoagulant tubes within seven days following symptom onset. Plasma was separated by centrifugation at 1,500 × g for 10 min, aliquoted, and stored at − 80 °C until subsequent biochemical, metabolomics, and lipidomics analyses.
Neutralizing antibody assay
A pseudovirus JN.1 strain of SARS-Cov-2 Omicron was constructed as described before39. A serum pseudovirus neutralization test was conducted by chemiluminescence method, and 50% neutralization dilution (ND50) level was calculated using the Reed-Muench method.
Cytokine and chemokine measurement
Plasma cytokine and chemokine profiles were determined using Bioplex Kit Assay (LINCO Research, Inc., USA) according to the manufacturer’s instructions.
Plasma metabolomics analyses
Plasma was separated from fasting venous blood and dried in a SpeedVac under H2O mode. The dried extract was reconstituted in 5% acetonitrile in water prior to LC-MS analysis on an Agilent 1290 II UPLC coupled to Sciex 5600 + quadrupole-TOF MS. For reverse phase chromatography, polar metabolites were separated on a Waters ACQUITY HSS-T3 column (3.0 × 100 mm, 1.8 μm). Data acquisition and processing were performed using Analyst® TF 1.7.1 Software (AB Sciex, Concord, ON, Canada). Metabolite quantitation was based on normalization of peak areas to their corresponding isotopically labeled structural analogues or optimized internal standards selected based on minimal coefficients of variation (COVs), as previously described40. Metabolite abundances were expressed as normalized peak areas.
Plasma lipidomics analyses
Lipids were extracted from plasma using a modified version of the Bligh and Dyer’s method as described previously40. Quantitative lipidomics was performed on a Jasper HPLC coupled with Sciex TRIPLE QUAD 4500 MD as reported previously28. Separation of individual lipid classes by normal phase (NP)-HPLC was carried out using a TUP-HB silica column (i.e. 150 × 2.1 mm, 3 μm). MRM transitions were set up for quantitative analyses of individual lipids, which were quantified by referencing to spiked internal standards. Detailed LC-MS/MS conditions and MRM transitions for targeted lipid classes including PC, PE, PI, PS, TAG, SM, SL, Cer, and FFAs are provided in the Supplementary Materials. Quantification was performed by referencing to spiked internal standards (e.g., d9-PC32:0, C17:0-LPC, d3-16:0 carnitine, TAG(16:0)₃-d5) obtained from Avanti, Sigma-Aldrich, CDN Isotopes, and Matreya.
Statistical analysis
Top 30 significantly differential lipids * P < 0.05, ** P < 0.01, ***P < 0.001 as determined by t-test were shown in the Circos plot. Over-representation analysis (ORA) of dysregulated pathways from the small molecule pathway database (SMPD) were performed based on differential metabolites conserved between Omicron infection and symptom severity. Total PE-Os across the different groups were shown as boxplot, pairwise comparisons using two-sided Games-Howell test was performed to determine the P values with letter-based representation where uncommon letter denoted statistical significance at P < 0.05.
To systematically interrogate changing lipid-metabolite coregulation, differential correlations between lipid-metabolite pairs in first infection (or reinfection) relative to healthy controls were calculated using the R package DGCA (v1.0.3). Correlation coefficients were converted into z-scores using Fisher’s z-transformation, and P values for differential correlations (pValDiff) between variables were calculated using differences in z-scores. Only significant lipid-metabolite pairs (pValDiff < 0.0001) were retained for the construction of global networks using the R package MEGENA (Multiscale Embedded Gene Co-Expression Network Analysis) (v1.3.7).
To examine metabolic pathway dysregulation specifically in first infection patients, ORA was performed on significantly altered metabolites (P < 0.05, t-test) exclusive to first infection patients relative to healthy participants using the KEGG database from R package “graphite”. Volcano plots of differential metabolites were constructed based on fold changes (FC >|1|) and P < 0.05 from t-test. Spearman correlation coefficients were calculated between the differential metabolites and lipid species between plasma indoles and PE-Osin Omicron-infected patients and L-histidine and top 30 differential TAGs amongst first infection Omicron patients and clinical parameters using the R package psych (v2.3.3), and significant correlations (P < 0.05) were illustrated as bubble plots. P < 0.05 was considered statistically significant.
Least absolute shrinkage and selection operator (Lasso) analysis were performed to determine the significant variables crucial for segregating the Omicron-infected patients according to severity. Controlling for age and gender as covariates, AUROC illustrated the prediction performance of these three variables. All statistical analyses were performed in R 4.2.3.
Detailed information is provided in Supplementary materials.
Limitations of the study
Our study remains cross-sectional, and longitudinal samples from the same patients at different timepoints were not collected to allow for paired comparisons of metabolic changes within an identical group of patients across repeated infections. The current sample size is reasonable but modest, and extrapolation of our findings to bigger cohorts of patients will be beneficial toward validating the reproducibility of the reported metabolic changes in patients of other ethnicities or geographical locations. Secondly, as samples were collected within a 7-day window from symptom onset, temporal variability may have been introduced. Some variability in the observed metabolomic patterns could be attributable to differences in sampling time across individuals. Thirdly, in the study, the proportion of male patients between 1st and repeated infected patients were comparable (p = 0.64). We could not exclude the impact of gender on metabolomics and lipidomics, which would be further dissected in future studies with large sample size. Finally, as omics per se is hypothesis generating in nature, the molecular pathobiology underlying the reported metabolic changes warrants future experimental validation in animal models or cell cultures.
Conclusions
In all, we identified systemic metabolic disturbances central to Omicron pathogenesis, which are likely modifiable by dietary intervention. Our findings also highlight the possibility of fine-tuning systemic immunity against Omicron (or other β-coronavirus) infections via modulating host-microbe interactions. For example, a high-protein or high-tryptophan diet may alter intestinal homeostasis via gut microbial-mediated indole production, or may change circulating histidine abundances by tilting the gut microbiome constitution of histidine utilizers. These may in turn modulate systemic inflammation and hepatic lipid production, which are crucial determinants of both the pathobiology and long-term sequelae of Omicron infections on host. In addition to host-microbe interactions, our findings also put forth specific lipid-centric intervention targets that may be useful against Omicron infections, including PLA2 and sulfatides. Considering the high mutation rates of specific coronavirus variants like the Omicron, and the problem of immune imprinting that puts constraints on vaccine efficacy, metabolism-focused approaches may present useful alternatives to boost community defense against continual waves of SARS-CoV-2 outbreaks.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Roemer, C. et al. SARS-CoV-2 evolution in the Omicron era. Nat. Microbiol. 8, 1952–1959. https://doi.org/10.1038/s41564-023-01504-w (2023).
Araf, Y. et al. Omicron variant of SARS-CoV-2: genomics, transmissibility, and responses to current COVID-19 vaccines. J. Med. Virol. 94, 1825–1832. https://doi.org/10.1002/jmv.27588 (2022).
Dyer, O. Covid-19: South africa’s surge in cases deepens alarm over Omicron variant. Bmj 375, n3013. https://doi.org/10.1136/bmj.n3013 (2021).
Shanmugaraj, B., Malla, A., Khorattanakulchai, N. & Phoolcharoen, W. SARS-CoV-2 Omicron variant: could it be another threat? J. Med. Virol. 94, 1284–1288. https://doi.org/10.1002/jmv.27532 (2022).
Uemura, K., Kanata, T., Ono, S., Michihata, N. & Yasunaga, H. The disease severity of COVID-19 caused by Omicron variants: A brief review. Ann. Clin. Epidemiol. 5, 31–36. https://doi.org/10.37737/ace.23005 (2023).
Garcia-Beltran, W. F. et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell 185, 457–466e454. https://doi.org/10.1016/j.cell.2021.12.033 (2022).
Paul, P. et al. Effectiveness of the pre-Omicron COVID-19 vaccines against Omicron in reducing infection, hospitalization, severity, and mortality compared to Delta and other variants: A systematic review. Hum. Vaccin Immunother. 19, 2167410. https://doi.org/10.1080/21645515.2023.2167410 (2023).
Tan, C. W. et al. Distinctive serotypes of SARS-related coronaviruses defined by convalescent Sera from unvaccinated individuals. Hlife 1, 26–34. https://doi.org/10.1016/j.hlife.2023.07.002 (2023).
Past, S. A. R. S. CoV-2 infection protection against re-infection: a systematic review and meta-analysis. Lancet 401, 833–842. https://doi.org/10.1016/s0140-6736(22)02465-5 (2023).
Diskin, C., Ryan, T. A. J. & O’Neill, L. A. Modification of proteins by metabolites in immunity. Immunity 54, 19–31. https://doi.org/10.1016/j.immuni.2020.09.014 (2021).
Balmer, M. L. et al. Memory CD8(+) T cells require increased concentrations of acetate induced by stress for optimal function. Immunity 44, 1312–1324. https://doi.org/10.1016/j.immuni.2016.03.016 (2016).
Ayres, J. S. A metabolic handbook for the COVID-19 pandemic. Nat. Metab. 2, 572–585. https://doi.org/10.1038/s42255-020-0237-2 (2020).
Li, X. et al. Plasma metabolomic characterization of SARS-CoV-2 Omicron infection. Cell. Death Dis. 14, 276. https://doi.org/10.1038/s41419-023-05791-3 (2023).
Wang, H. et al. Multi-omics blood atlas reveals unique features of immune and platelet responses to SARS-CoV-2 Omicron breakthrough infection. Immunity 56, 1410–1428e1418. https://doi.org/10.1016/j.immuni.2023.05.007 (2023).
Lam, S. M. et al. A robust, integrated platform for comprehensive analyses of acyl-coenzyme as and acyl-carnitines revealed chain length-dependent disparity in fatty acyl metabolic fates across Drosophila development. Sci. Bull. (Beijing). 65, 1840–1848. https://doi.org/10.1016/j.scib.2020.07.023 (2020).
Lam, S. M., Wang, Z., Li, B. & Shui, G. High-coverage lipidomics for functional lipid and pathway analyses. Anal. Chim. Acta. 1147, 199–210. https://doi.org/10.1016/j.aca.2020.11.024 (2021).
Song, J. W. et al. Omics-Driven systems interrogation of metabolic dysregulation in COVID-19 pathogenesis. Cell. Metab. 32, 188–202e185. https://doi.org/10.1016/j.cmet.2020.06.016 (2020).
Losol, P. et al. A cross talk between microbial metabolites and host immunity: its relevance for allergic diseases. Clin. Transl Allergy. 14, e12339. https://doi.org/10.1002/clt2.12339 (2024).
Sanchez, E. L. & Lagunoff, M. Viral activation of cellular metabolism. Virology 479–480, 609–618. https://doi.org/10.1016/j.virol.2015.02.038 (2015).
Liberti, M. V. & Locasale, J. W. The Warburg effect: how does it benefit Cancer cells?? Trends Biochem. Sci. 41, 211–218. https://doi.org/10.1016/j.tibs.2015.12.001 (2016).
Heer, C. D. et al. Coronavirus infection and PARP expression dysregulate the NAD metabolome: an actionable component of innate immunity. J. Biol. Chem. 295, 17986–17996. https://doi.org/10.1074/jbc.RA120.015138 (2020).
Alexeev, E. E. et al. Microbial-derived Indoles inhibit neutrophil myeloperoxidase to diminish bystander tissue damage. Faseb J. 35, e21552. https://doi.org/10.1096/fj.202100027R (2021).
Amunugama, K. et al. Identification of novel neutrophil very long chain plasmalogen molecular species and their myeloperoxidase mediated oxidation products in human sepsis. Redox Biol. 48, 102208. https://doi.org/10.1016/j.redox.2021.102208 (2021).
Albert, C. J., Crowley, J. R., Hsu, F. F., Thukkani, A. K. & Ford, D. A. Reactive chlorinating species produced by myeloperoxidase target the vinyl ether bond of plasmalogens: identification of 2-chlorohexadecanal. J. Biol. Chem. 276, 23733–23741. https://doi.org/10.1074/jbc.M101447200 (2001).
Danne, C., Skerniskyte, J., Marteyn, B. & Sokol, H. Neutrophils: from IBD to the gut microbiota. Nat. Rev. Gastroenterol. Hepatol. 21, 184–197. https://doi.org/10.1038/s41575-023-00871-3 (2024).
Liu, Y. et al. Indole metabolites and colorectal cancer: gut microbial Tryptophan metabolism, host gut Microbiome biomarkers, and potential intervention mechanisms. Microbiol. Res. 272, 127392. https://doi.org/10.1016/j.micres.2023.127392 (2023).
Yeoh, Y. K. et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut 70, 698–706. https://doi.org/10.1136/gutjnl-2020-323020 (2021).
Lam, S. M. et al. A multi-omics investigation of the composition and function of extracellular vesicles along the Temporal trajectory of COVID-19. Nat. Metab. 3, 909–922. https://doi.org/10.1038/s42255-021-00425-4 (2021).
Snider, J. M. et al. Group IIA secreted phospholipase A2 is associated with the pathobiology leading to COVID-19 mortality. J. Clin. Invest. 131 https://doi.org/10.1172/jci149236 (2021).
Barcik, W., Wawrzyniak, M., Akdis, C. A. & O’Mahony, L. Immune regulation by Histamine and Histamine-secreting bacteria. Curr. Opin. Immunol. 48, 108–113. https://doi.org/10.1016/j.coi.2017.08.011 (2017).
Conti, P. et al. Mast cells activated by SARS-CoV-2 release Histamine which increases IL-1 levels causing cytokine storm and inflammatory reaction in COVID-19. J. Biol. Regul. Homeost. Agents. 34, 1629–1632. https://doi.org/10.23812/20-2edit (2020).
Metcalfe, D. D. et al. Biomarkers of the involvement of mast cells, basophils and eosinophils in asthma and allergic diseases. World Allergy Organ. J. 9. https://doi.org/10.1186/s40413-016-0094-3 (2016).
Quesada-Vázquez, S. et al. Potential therapeutic implications of histidine catabolism by the gut microbiota in NAFLD patients with morbid obesity. Cell. Rep. Med. 4, 101341. https://doi.org/10.1016/j.xcrm.2023.101341 (2023).
Dinarello, C. A. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol. Rev. 281, 8–27. https://doi.org/10.1111/imr.12621 (2018).
Barcia, A. M. & Harris, H. W. Triglyceride-rich lipoproteins as agents of innate immunity. Clin. Infect. Dis. 41 (Suppl 7), S498–503. https://doi.org/10.1086/432005 (2005).
Bao, X. & Wu, J. Impact of food-derived bioactive peptides on gut function and health. Food Res. Int. 147, 110485. https://doi.org/10.1016/j.foodres.2021.110485 (2021).
Scott, J. D. & Williams, R. M. Chemistry and biology of the tetrahydroisoquinoline antitumor antibiotics. Chem. Rev. 102, 1669–1730. https://doi.org/10.1021/cr010212u (2002).
Toelzer, C. et al. The free fatty acid-binding pocket is a conserved hallmark in pathogenic β-coronavirus Spike proteins from SARS-CoV to Omicron. Sci. Adv. 8, eadc9179. https://doi.org/10.1126/sciadv.adc9179 (2022).
Yu, X. et al. Three doses of an inactivation-based COVID-19 vaccine induces cross-neutralizing immunity against the SARS CoV-2 Omicron variant. Emerg. Microbes Infect. 11, 749–752. https://doi.org/10.1080/22221751.2022.2044271 (2022).
Miao, H. et al. Lipidome atlas of the developing heart uncovers dynamic membrane lipid attributes underlying cardiac structural and metabolic maturation. Research (Wash D C). 0006 (2022). https://doi.org/10.34133/research.0006 (2022).
Acknowledgements
This work was supported by the National Key R&D Program of China (#2023YFC0872400 and #2022YFE0102300 to Yingmei Feng and #2023YFC3043502 to Jiaying Zhang). We thank Dr. Wei Ling Florence Lim for her professional language editing. We thank Ning Liu, Ying Wang, Xuanyi Yang and Jihui Jia for blood sample collection and preparation.
Author information
Authors and Affiliations
Contributions
J.Z., S.L., Sh. J., L.Zh., J.Y., H.S., and D.M. collected the samples and performed experiments. Q.M., G.Sh., and Y.F. designed the study and analyzed the data. S.L.and Y.F. wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, J., Lam, S.M., Ji, S. et al. Metabolic features of patients with repeated Omicron infections highlight new targets for therapeutic intervention. Sci Rep 15, 22134 (2025). https://doi.org/10.1038/s41598-025-04745-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-04745-3