Abstract
Previous studies have indicated increased dementia risk associated with fine particulate matter (PM2.5) exposure; however, the findings are inconsistent. In this systematic review, we assessed the association between long-term PM2.5 exposure and dementia outcomes using the Burden of Proof meta-analytic framework, which relaxes log-linear assumptions to better characterize relative risk functions and quantify unexplained between-study heterogeneity (PROSPERO, ID CRD42023421869). Here we report a meta-analysis of 28 longitudinal cohort studies published up to June 2023 that investigated long-term PM2.5 exposure and dementia outcomes. We derived risk–outcome scores (ROSs), highly conservative measures of effect size and evidence strength, mapped onto a 1–5-star rating from ‘weak and/or inconsistent evidence’ to ‘very strong and/or consistent evidence’. We identified a significant nonlinear relationship between PM2.5 exposure and dementia, with a minimum 14% increased risk averaged across PM2.5 levels between 4.5 and 26.9 µg m−3 (the 15th to 85th percentile exposure range across included studies), relative to a reference of 2.0 µg m−3 (n = 49, ROS = 0.13, two stars). We found a significant association of PM2.5 with Alzheimer’s disease (n = 12, ROS = 0.32, three stars) but not with vascular dementia. Our findings highlight the potential impact of air pollution on brain aging.
Similar content being viewed by others
Main
Given the increase in the aging population worldwide1, dementia has emerged as a pressing public health issue. The 2021 Global Burden of Diseases, Injuries and Risk Factors Study (GBD) highlights dementia as the fifth leading cause of death and disability in 2021 among individuals aged 75 years and older, accounting for 1.66 million deaths (95% uncertainty interval (UI) 0.44–4.27), 36.4 million prevalent cases (30.9–42.7) and 25.3 million disability-adjusted life-years (11.7–53.6) globally2,3. With nearly 10 million new cases estimated each year, the World Health Organization (WHO) projects that the total number of people living with dementia will reach 152 million by 2050 (ref. 4).
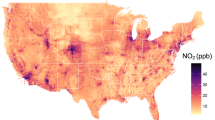
Air pollution, especially fine particulate matter with a diameter ≤2.5 μm (PM2.5), has been identified as a potential risk factor for cognitive decline and dementia, with pathological and epidemiological studies supporting a plausible risk–outcome relationship5,6,7,8,9,10. With more than 90% of the global population exposed to annual PM2.5 concentrations exceeding the WHO air quality guideline of 5 μg m−3, the majority of individuals may face an elevated risk of dementia11. The Dementia Prevention, Intervention and Care report issued by the Lancet Commission in 2024 included air pollution as one of 14 modifiable risk factors for dementia, suggesting a weighted population attributable fraction (PAF; the proportional reduction in dementia risk that would occur if PM2.5 exposure were reduced to the theoretical minimum exposure level) of 2.6% (ref. 12); however, this estimated PAF was based on a single epidemiologic study and did not incorporate the spectrum of emerging evidence for effect estimates available in the recent literature.
Recent meta-analyses evaluating the epidemiological evidence of the PM2.5–dementia relationship indicate an adverse impact of elevated exposure levels, although with substantial variation in effect magnitudes across studies. Abolhasani et al. estimated a 3% (95% confidence interval (CI) 2–5) increase in dementia risk per 1 μg m−3 PM2.5 increase based on 14 studies8, while Cheng et al. reported a pooled hazard ratio (HR) of 1.03 (CI 1.02–1.05) for dementia per 1 μg m−3 increment of PM2.5 based on 18 studies10. Wilker et al. found an adverse but not significant impact of PM2.5 on dementia with an HR of 1.02 (CI 0.99–1.04) per 1 μg m−3 PM2.5 increase13. A few meta-analytical studies also attempted to evaluate the specific impact of PM2.5 on the two most common dementia subtypes of Alzheimer’s disease (AD) and vascular dementia (VaD). Cheng et al. reported a 4% (CI 2–6) elevated risk of AD per 1 μg m−3 increment of PM2.5 based on 13 studies10, while another meta-analysis found a nonsignificant impact of PM2.5 on AD across nine studies14. For VaD, one meta-analysis of eight cohort studies reported an HR of 1.07 (CI 1.03–1.12) per 1 μg m−3 PM2.5 (ref. 10).
However, existing meta-analytical literature on PM2.5 and dementia suffer from several limitations. Common meta-analytical frameworks, such as linear mixed-effect models, have been criticized as being overly simplistic, lacking appropriate bias assessment and unable to reflect the typically complex shape of risk–outcome relationships involving air pollution15,16,17. Furthermore, in traditional statistical approaches, between-study heterogeneity that is not explained by known differences in study-level characteristics is usually not adequately considered or quantitively assessed16.
In this study, we implemented the Burden of Proof framework recently developed by Zheng et al.16,18 to estimate the continuous dose–response relationship of ambient PM2.5 and dementia, including all types of dementia and specific subtypes such as AD and VaD. Notably, the method relaxes the conventional (log-)linear assumption for the relative risk (RR) curve, offering the flexibility required for optimal data fitting. It also provides a means to incorporate unexplained between-study heterogeneity into estimates of uncertainty after accounting for known variation in study design characteristics, in addition to accounting for small numbers of studies. The method also allows us to derive the Burden of Proof Risk Function (BPRF), which can be interpreted as the lowest, most conservative estimate of excess dementia risk associated with PM2.5 exposure, based on the available evidence. To facilitate interpretation and comparability, the BPRF, which incorporates both the strength of risk–outcome associations and the consistency of their underlying evidence, is translated into a risk–outcome score (ROS) and associated star rating, ranging from one star (weak and/or inconsistent evidence of an association) to five stars (very strong and/or consistent evidence of an association)18. The main findings and policy implications of this study are presented in Table 1.
Results
Overview
We systematically searched the literature for studies assessing the impact of long-term PM2.5 exposure on dementia risk, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines19. We initially identified the most recent peer-reviewed systematic review that complied with PRISMA guidelines, namely, a study by Wilker et al.13 that spanned the periods from the inception of each database searched to July 2022. To generate an updated systematic review, we employed search strings in alignment with those used in Wilker et al.13 and searched PubMed, Embase and Web of Science to further identify studies published between July 2022 and June 2023 (Extended Data Fig. 1). Our search initially identified 38 papers reviewed in Wilker et al.13, which we supplemented with an additional 21 papers retrieved from the database search. After evaluation, we excluded 31 papers that did not meet our inclusion criteria. (The search terms and inclusion/exclusion criteria are outlined in the Supplementary Information and the detailed inclusion/exclusion decisions and rationale for each study are provided in Supplementary Table 4). In total, we integrated data from 28 longitudinal cohort studies20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47, which contributed a collective total of 49 HRs to our meta-regression analysis. More specifically, we incorporated 26 HRs21,22,23,24,25,26,27,28,30,31,33,34,35,36,37,38,39,40,42,43,45,46,47 for all-cause dementia outcomes, 12 HRs20,22,25,28,30,31,32,34,40,41,43,44 for AD outcomes, six HRs22,24,25,28,40,43 for VaD outcomes and five HRs22,25,29,30,31 for other types of dementia (Extended Data Fig. 1).
Collectively, the studies included in our meta-analysis comprised 11 cohort studies conducted in Europe, nine in the United States, four in China, three in Canada and one in Australia (Supplementary Table 5). The aggregated data included approximately 2.73 million incident dementia cases and dementia mortalities, which were derived from a total population of 36.3 million individuals. The duration of follow-up varied among the studies, ranging from 3 to 25 years, with a median of 13 years (interquartile range (IQR) 9–15 years). Estimated long-term ambient PM2.5 exposure levels exhibited considerable variability, ranging from 0.1 to 61.7 µg m−3 PM2.5 across the entire participant pool. Detailed study characteristics are in Supplementary Table 5. Extended Data Fig. 2 provides the extracted HR from each included study for all-cause dementia, AD, VaD and other types of dementia, all scaled for a standard PM2.5 increment of 1 µg m−3. The meta-analytic results, including effect estimates, key analytic parameters and characteristics of the PM2.5–dementia relationship, in addition to results from analysis restricted to dementia subtypes (AD and VaD), are presented in Table 2.
PM2.5 and dementia
Our main meta-regression—Bayesian, regularized, trimmed (MR-BRT) model (Methods) for all dementia outcomes combined revealed a statistically significant relationship between ambient PM2.5 exposure and dementia risk. We found a consistent increase in the risk of dementia incidence and mortality across the exposure range (Fig. 1 and Supplementary Table 7). Notably, our analysis delineated a monotonically increasing curve characterizing this association, indicating a considerable rise in risk until PM2.5 levels reached approximately 15 µg m−3, followed by a more modest risk increase at higher PM2.5 levels. At the observed mean PM2.5 exposure level of 15.5 µg m−3 across all included studies, the mean RR of dementia was 1.37 (95% UI inclusive of between-study heterogeneity 1.13–1.69), compared to the reference PM2.5 exposure of 2.0 µg m−3 (Table 2). The reference PM2.5 exposure in our study represents the lowest observed reference level across all the included studies.
a, RR function. The solid green line represents the mean RR at each exposure level, and the solid red line represents the BPRF. The dark green shaded area indicates the 95% UI without accounting for between-study heterogeneity, and the light green shaded area represents the 95% UI accounting for between-study heterogeneity. The size of the data points is proportional to the inverse of the s.d. of the effect estimates, where larger points indicate higher precision in the effect estimates. b, A modified funnel plot showing the residuals (relative to zero) on the x axis and the estimated s.d. (inclusive of between-study heterogeneity) on the y axis.
In our conservative BPRF-based assessment of the evidence, which complements conventional RR estimates, the BPRF is defined for harmful risks as the fifth percentile estimated risk curve inclusive of between-study heterogeneity that is closest to the null16,18, illustrated by the red line in Fig. 1a. The exposure-averaged BPRF of 1.14 demonstrates that ambient PM2.5 exposure in the range of the 15th percentile to 85th percentile (PM2.5, 4.5–26.9 µg m−3) elevates the risk of dementia by at least 14% on average, relative to a reference value of 2.0 µg m−3. The estimated harmful association between PM2.5 and dementia, as indicated by the corresponding ROS (the signed value of the log exposure-averaged BPRF) of 0.13, corresponds to a two-star rating (Table 2).
Accounting for study bias and quantifying heterogeneity
Among the 12 candidate covariates identified based on six primary sources of bias, per Grading of Recommendations, Assessment, Development and Evaluations (GRADE) criteria48, including representativeness of the study population, exposure measurement, outcome assessment, potential for reverse causation, control for confounding variables and selection bias (step 3 of Methods and Supplementary Table 6), only the covariate representing the AD outcome (1 for AD outcomes, 0 for non-AD outcomes) was found to have a significant effect on the RR curve and therefore included as a covariate in the final model for all dementia outcomes combined. In a separate step, we used a Fisher information matrix49 to quantify any remaining unexplained heterogeneity and integrated this estimate into uncertainty intervals. Our analysis revealed a sustained level of moderate unexplained between-study heterogeneity within our set of included studies, evident from the 95% UI inclusive of between-study heterogeneity for the RR curve, as illustrated in light blue shades in Fig. 1a.
Our analysis additionally uncovered evidence of publication bias, supported by a significant P value (0.03) derived from the Egger’s regression test50. The asymmetry evident in the funnel plot (Fig. 1b) illustrates a skewed distribution, notably with a clustering of data predominantly on the right side, where the residual is larger than zero. This imbalance suggests a propensity for studies with notably positive results to be more prominently featured within the published literature. The Supplementary Information contains detailed results for our assessment of study quality and risk of bias.
Subgroup analysis
We conducted subgroup analyses specifically focusing on the association between PM2.5 exposure and AD and VaD outcomes, depicted by the risk curves in Figs. 2a and 3a, respectively. We included 12 studies for AD and six studies for VaD and (unlike the approach we took for the full dementia analysis) did not trim the data for outliers due to the limited datasets for studies for dementia subtypes (Extended Data Fig. 1 and Supplementary Table 5). Our findings indicated a significant association between elevated PM2.5 exposure and the risk of AD (Fig. 2a). At the mean exposure level of 15.5 µg m−3, the mean RR for AD was estimated to be 1.39 (95% UI inclusive of between-study heterogeneity 1.33–1.44) compared to the reference PM2.5 level (Table 2). It is noteworthy that even when including between-study heterogeneity, the 95% UI remained remarkably narrow. On average, as indicated by an estimated BPRF of 1.38, AD increased by at least 38% for populations exposed to PM2.5 levels between the 15th and 85th percentile (5.0–40.7 µg m−3) as compared to those exposed to a reference level of 2.0 µg m−3. The ROS for PM2.5 exposure and AD outcomes was 0.32, representing a three-star rating risk–outcome pair. Conversely, while the mean VaD risk tended to rise with increased PM2.5 exposure, our analysis did not find a significant association (Fig. 3a and Table 2). The notably wide 95% UI indicated that the PM2.5–VaD relationship was characterized by a high degree of uncertainty and sensitivity. For detailed estimates of risks of both AD and VaD in response to PM2.5 exposure, including their corresponding 95% UI inclusive of heterogeneity, refer to Supplementary Tables 8 and 9. We observed significant publication bias for AD (P = 0.04) but not for VaD.
a, RR function. The solid green line represents the mean RR at each exposure level, and the solid red line represents the BPRF. The dark green shaded area indicates the 95% UI without accounting for between-study heterogeneity, while the light green shaded area represents the 95% UI accounting for between-study heterogeneity. The size of the data points is proportional to the inverse of the s.d. of the effect estimates, where larger points indicate higher precision in the effect estimates. b, A modified funnel plot showing the residuals (relative to zero) on the x axis and the estimated s.d. (inclusive of between-study heterogeneity) on the y axis.
a, RR function. The solid green line represents the mean RR at each exposure level. The dark green shaded area indicates the 95% UI without accounting for between-study heterogeneity, while the light green shaded area represents the 95% UI accounting for between-study heterogeneity. The size of the data points is proportional to the inverse of the s.d. of the effect estimates, where larger points indicate higher precision in the effect estimates. b, A modified funnel plot showing the residuals (relative to zero) on the x axis and the estimated s.d. (inclusive of between-study heterogeneity) on the y axis.
Stratified and sensitivity analyses
We conducted three sensitivity analyses to examine variations in potential PM2.5–dementia associations. First, stratified analysis by dementia case diagnosis revealed stronger evidence for an association in the ten included studies using active ascertainment of dementia cases (ROS = 0.23, three-star) compared to those (18 studies) relying on passive diagnosis or self-reported cases (ROS = 0.04, two-star) (Extended Data Figs. 3 and 4). Second, in a subset of 15 studies restricted to older adults with a baseline age ≥60 years, we observed a three-star association (ROS = 0.19), showing stronger evidence compared to the 13 included studies including participants with a broader baseline age range (ROS < 0, one star) (Extended Data Figs. 5 and 6). Third, subregion analyses indicated a two-star association (ROS = 0.001) among 12 studies conducted in North America, whereas no consistent evidence was found for 11 studies conducted in Europe (Extended Data Figs. 7 and 8). Due to limited data availability, subregion analyses were not performed for other regions. Notably, the stratified analyses for studies using active ascertainment and for the older adults both showed stronger evidence compared to the overall association observed in the main analysis (ROS = 0.13, two-star).
To test the model fitting and robustness, we further implemented two alternative models without trimming and with 15% trimming. Comparing the mean risk curves estimated from these two models to the main model for all dementia outcomes combined that employed 10% trimming, no significant differences were found (Supplementary Fig. 1). Even when including outliers without trimming, the estimated association between ambient PM2.5 and dementia risk remained significant. However, a noticeably wider 95% UI inclusive of between-study heterogeneity was evident. Both alternative models retained a two-star rating, but the estimated ROS was lower compared to the main model, with an ROS of 0.14 for the 15%-trimming model and 0.08 for the no-trimming model. Furthermore, we conducted sensitivity analyses to investigate the influence of adjusting the monotonicity constraint and utilizing cubic splines on the estimated risk curves. Notably, the removal of enforced model shape constraints did not yield substantial alterations in the risk curve outcomes for all-type dementia and AD (Supplementary Fig. 1 and Figs. 2 and 3). However, the risk curves related to VaD demonstrated pronounced sensitivity to these specific constraints (Supplementary Fig. 1 and Figs. 2 and 3).
Discussion
Our study systematically reviewed 28 cohort studies providing 49 effect estimates characterizing the relationship between long-term ambient PM2.5 exposure and dementia. Using the Burden of Proof meta-analytical framework, we constructed flexible RR functions that did not presume a (log-)linear relationship, demonstrating a significant association between increased PM2.5 exposure levels and heightened risks of all dementia outcomes combined. The estimated RR curve indicates a notably steeper rise in dementia risk at lower PM2.5 levels before reaching the mean exposure level across all included studies, approximately 15 µg m−3. Beyond this point, the rise in RR with increasing PM2.5 exposure becomes much less steep. Based on the conservative BPRF metrics our method generates in conjunction with the RR function, we estimated a minimum average increase in dementia risk of 14% associated with ambient PM2.5 exposure between 4.5 and 26.9 µg m−3 (relative to a reference level of 2.0 µg m−3). The two-star rating, derived from an ROS of 0.13, is interpreted in the Burden of Proof framework as indicating weak evidence of an association, based on the available data.
Our subtype analysis highlights that PM2.5 exposure may impact dementia risk differently across subtypes. AD, as represented by a binary covariate, proved to be significant in the overall PM2.5–dementia analysis; it was the only significant covariate identified by our algorithm from a set of 12 covariates. When conducting subtype-specific meta-regression, our conservative BPRF metrics indicated a significant relationship between PM2.5 and AD, yielding a three-star rating (ROS = 0.32), indicating a moderate association and/or moderately consistent evidence given the available data. Our study demonstrated stronger evidence for the PM2.5–AD relationship compared to the association between PM2.5 and all dementia outcomes combined (two stars). Notably, the 95% UI around the RR function for AD is very narrow, even when incorporating unexplained between-study heterogeneity, which at least partially explains the finding that the evidence for the PM2.5–AD relationship is relatively strong. Meanwhile, based on a limited number of studies (n = 6), we did not observe a significant relationship between VaD and PM2.5 exposure, however, the mean effect of PM2.5 suggests there may be an increase in VaD risk. Figure 2a illustrates the considerable heterogeneity in effect estimates for VaD that likely underlie the large uncertainty estimates. This heterogeneity is partly driven by one study, which reported a significantly higher effect estimate with greater uncertainty, based on an analysis with only 70 VaD cases among 2,927 participants24. With VaD comprising 10–20% of dementia cases compared to 40–60% for AD51,52, its lower incidence likely reduces the power of the statistical analysis and amplifies the uncertainty in the results. Another major source of heterogeneity stems from the clinical diagnosis of dementia subtypes. It is common that information regarding dementia subtype diagnosis is inaccurate or missing, particularly when relying on passive ascertainment, leading to potential under-reporting and misclassification53,54; most of the subtype studies included (7 out of 12 for AD, and 5 out of 6 for VaD) used administrative medical records or death certificates. Furthermore, as observed in recent neuropathological studies55,56, AD, VaD, and other dementia subtypes may display a co-occurrence of multiple neuropathological hallmarks, indicating that current clinical diagnoses of dementia subtypes are an imperfect science and may not always reflect all underlying brain pathologies accurately. Possible misclassification or over-classifications may have introduced potential biases into our subgroup analyses.
The findings from our stratified analyses highlight the influence of dementia diagnosis methods, population characteristics, and regional differences on the estimated PM2.5–dementia associations. Stratified analysis by diagnosis methods revealed stronger evidence for an association in studies using active ascertainment through physician diagnosis (ROS = 0.23, three stars) compared to those relying on passive ascertainment via medical records, death certificates or self-reports (ROS = 0.04, two stars). These results align with a previous meta-analysis of PM2.5 and dementia, which reported significant associations only in studies employing active ascertainment, with no significant findings in studies using passive ascertainment methods13. The weaker associations observed in studies with passive ascertainment or self-reports are likely biased toward the null due to a higher risk of outcome misclassification or underdiagnosis in these methods compared to active ascertainment57. Analysis restricted to studies involving older adults (baseline age ≥60 years) revealed stronger evidence for the association between PM2.5 exposure and dementia (ROS = 0.19, three stars), compared to the main analysis including all studies (ROS = 0.13, two stars). The higher mean RR observed among the older adults focused studies suggests that older individuals may be more vulnerable to PM2.5 exposure, potentially due to increased susceptibility linked to age-related declines in physiological resilience and greater pre-existing health risks, amplifying PM2.5-related dementia risk58. Subregional analyses showed weaker evidence for PM2.5–dementia associations in studies conducted in North America (ROS = 0.001, one star) and no significant evidence in Europe, compared to the main analysis. These regional variations may reflect differences in PM2.5 sources, composition and exposure levels59,60, as well as population characteristics, socioeconomic factors and variability in dementia diagnostic methods across regions61.
Our study findings corroborate the positive association between PM2.5 exposure and dementia, which is supported by neuropathological studies demonstrating a biologically plausible effect of ambient PM2.5 on dementia risk5,6,7. PM2.5, particularly nanoscaled particles, can penetrate the human brain via two primary pathways: a direct route through the olfactory nerve, and an indirect route through the circulation system that crosses the blood–brain barrier6,62,63,64,65. Once entering the brain, PM2.5 has the potential to increase neurological oxidative stress, neuroinflammation, neurotoxicity, neurovascular damage and impairment of the blood–brain barrier and brain cells5,6,7,66,67,68,69. Through the systemic pathway, PM2.5 may even cause systemic oxidative stress and inflammation, thereby contributing to the progression of dementia62,70. In addition, epidemiological and clinical evidence has linked PM2.5 exposure to heightened cardiovascular disease risks, including conditions like hypertension and atherosclerosis71,72. These cardiovascular conditions may adversely impact cerebral blood flow and compromise neurovascular function, potentially elevating the risk of developing dementia73. Moreover, in the context of AD risk, other potential mechanisms involving PM-induced modifications in AD-related genes through DNA methylation, coupled with an elevated risk of brain amyloid-β deposition and tau protein neurofibrillary tangles, have been suggested in the literature74,75. Collectively, these factors contribute to a heightened risk of neurodegeneration, cognitive decline and the onset of dementia.
Our study has several key advantages over previous meta-analyses evaluating the relationship between PM2.5 exposure and dementia risk. First, it incorporated a greater number of individual studies and effect estimates than did previous meta-analyses. Second, the Burden of Proof analysis framework relaxes the (log-)linear assumptions common to traditional random effects models, allowing the implementation of flexible splines with monotonicity constraints. Moreover, our methodology involves a robust process for identifying and trimming outliers within the dataset to mitigate the impact of the inconsistency from existing literature. Notably, our conservative BPRF metrics incorporate unexplained between-study heterogeneity remaining after testing predefined bias covariates from a candidate set consistent with GRADE48 and Cochrane76 criteria and including significant covariates in the model, thus reducing the risk of spurious significant associations.
Additionally, our analysis provides an ROS and overarching star rating for the PM2.5–dementia relationships examined, facilitating a more intuitive assessment of the strength of evidence and comparison with other Burden of Proof evaluations of risk–outcome relationships involving dementia or air pollution. In comparison to other risk factors evaluated for associations with dementia included in recent GBD studies, namely, smoking (ROS = 0.09, two stars), high fasting plasma glucose (ROS = 0.04, two stars), and high body mass index (ROS = −0.07, one star), we estimated a higher ROS for PM2.5–dementia (ROS = 0.13, two stars)77,78. Additionally, when considering PM2.5 exposure-related risk–outcome relationships investigated in the current GBD analyses, the PM2.5–dementia association is weaker than that for PM2.5 and chronic obstructive pulmonary disease (ROS = 0.44, four stars); tracheal, bronchus and lung cancer (ROS = 0.34, three stars); ischemic heart disease (ROS = 0.26, three stars); diabetes mellitus type 2 (ROS = 0.19, three stars); stroke (ROS = 0.17, three stars); and lower respiratory infections (ROS = 0.15, three stars)77. The ROSs and star ratings for all risk–outcome pairs analyzed using the Burden of Proof framework and BPRF metrics are further accessible online through the Burden of Proof online visualization tool (https://vizhub.healthdata.org/burden-of-proof/).
Our ability to estimate a nonlinear dose–response function, as afforded by our flexible Burden of Proof methods, revealed that even at relatively low exposure levels (<15 µg m−3), there is a rapidly increasing risk of dementia with increasing ambient PM2.5 exposure. This finding underscores the urgency and necessity for policymakers to adjust air quality regulations to reduce air pollution levels that can negatively impact human brain health and healthy aging. The current WHO air quality guideline (AQG) recommends that the annual PM2.5 exposure concentration should not exceed 5 µg m−3 (ref. 79); however, existing national or regional air quality policies with legal enforcement are generally less stringent than the WHO AQG. For instance, the US National Ambient Air Quality Standards set the annual mean PM2.5 limit at 9 µg m−3 (ref. 80); Australia’s standard is 8 µg m−3 (ref. 81); and Canada’s is 8.8 µg m−3 (ref. 82). The United Kingdom aims to meet a 10 µg m−3 standard by 2040 (ref. 83). The European Union’s stage-two standard is currently 20 µg m−3 (ref. 84); however, a provisional political agreement was reached in February 2024 to lower this to 10 µg m−3 by 2030 (ref. 85). Japan’s standard is 15 µg m−3 (ref. 86), while China allows up to 35 µg m−3 (ref. 87). Given that more than 90% of people live in areas where PM2.5 levels exceed the WHO AQG guideline11, there is a pressing need for updated policies and adequate enforcement of air pollution regulations to reduce ambient PM2.5 exposure globally. Our findings can help raise public awareness about the adverse impacts of air pollution on dementia risk, thereby supporting the development and adoption of stricter air quality regulations. Effective policy adjustments are crucial for mitigating the health risks associated with PM2.5 exposure and safeguarding public health, particularly in terms of human brain health outcomes.
Our study is constrained by several limitations related to both input data and the modeling approach. Concerning input data, our meta-analysis is limited by the small number of published studies; in particular, constraining our subtype analysis, which included 12 studies for AD and 6 studies for VaD. Additionally, we were unable to perform meta-analyses for other dementia subtypes, such as senile dementia, frontotemporal dementia and Lewy body dementia, due to the scarcity or absence of relevant longitudinal epidemiological studies. Furthermore, the dataset displays a geographical imbalance, with input studies heavily concentrated in North America, Europe and Asia, potentially limiting global representation. Moreover, our analysis focuses exclusively on ambient PM2.5 exposure, without assessing the potential impacts of other air pollutants, such as O3 and NO2. Nor did we explore the potential combined effects of multiple pollutants on dementia risk due to the limited data availability, with only four studies accounting for PM2.5 and O3 combined effects20,34,38,47 and four on PM2.5 and NO2 combined effects27,34,38,47. Future research on both the individual effects of other pollutants besides PM2.5 on dementia risk as well as their joint impacts to provide a more comprehensive understanding of how air pollution contributes to dementia. In terms of the modeling approach, it is possible that our framework, despite the application of rigorous statistical methods, may not comprehensively address all potential sources of heterogeneity and bias. Although we attempted to account for known variation in study characteristics through comprehensive bias covariates, such bias might not be captured and corrected in the final model if all or the majority of the input studies are biased.
In conclusion, applying the Burden of Proof framework of Zheng et al.16, our systematic meta-analysis found a significant association between ambient PM2.5 exposure and dementia, deriving nonlinear RR curves from 28 epidemiological cohort studies available up to June 2023. Despite a moderate degree of between-study heterogeneity within the existing evidence, our synthesis revealed a weak association between PM2.5 exposure and dementia. For subtype analyses, a stronger association emerged between ambient PM2.5 and AD outcomes supported by moderate evidence (three stars), whereas no consistent evidence of an association across reviewed studies was found for VaD. Our meta-analytic assessments of the impact of long-term exposure to ambient PM2.5 on dementia yield useful data for stakeholders including policymakers, public health professionals and the general public. These insights can be used to inform policy formation and advance the protection and enhancement of human brain health through improved air pollution management.
Methods
Overview
This meta-analysis is based on the recently developed ‘Burden of Proof’ framework published by Zheng et al.16,18, and the implementations are disseminated using open-source Python libraries88,89. We used the MR-BRT model, a meta-analytic tool utilizing Bayesian regularized splines, to estimate the dose–response risk curves for long-term ambient PM2.5 exposure and dementia, relaxing the assumption of a log(linear) relationship. In addition, we conservatively estimated the BPRF for the risk–outcome association incorporating between-study heterogeneity to evaluate the strength of evidence across the included studies supporting the association. The ‘Burden of Proof’ framework has been employed to assess health effects associated with other risk factors90,91,92,93,94,95,96,97. This meta-analytic methodology consists of six main steps: (1) conduct a systematic review and extract data from identified studies reporting on the association between long-term ambient PM2.5 exposure and dementia using a GBD-standardized systematic review protocol; (2) estimate the continuous risk–outcome relationship, using the minimum exposure level among all included studies as the reference; (3) test and adjust for systematic biases as a function of known input study attributes; (4) quantify remaining unexplained between-study heterogeneity while adjusting for within-study correlation induced by computing the RRs for several alternatives with the same reference, as well as the number of studies; (5) assess evidence for small-study effects to evaluate potential risk of publication or reporting bias; and (6) estimate the BPRF, which provides a conservative measure of the average risk increase across the range of exposure supported by the evidence and is to compute the ROS, and subsequently map the ROS into five categories of star ratings.
The estimates for our primary indicators from this work (RRs across a range of exposures, BPRFs, ROSs and star ratings for ambient PM2.5 and dementia outcomes) are not specific to or disaggregated by specific populations (we did not estimate by ___location, sex or age group; and this analysis evaluated the effects of long-term exposure to PM2.5 on dementia in adults 30 years and older only); however, we did include studies that were conducted in female-only populations.
We followed PRISMA guidelines19 (Supplementary Tables 10 and 11 and Extended Data Fig. 1) and Guidelines on Accurate and Transparent Health Estimates Reporting recommendations98 (Supplementary Table 12) for reporting our methods and analyses. This systematic review was registered as a systematic review in the International Prospective Register of Systematic Reviews (PROSPERO, ID CRD42023421869). This study was approved by the University of Washington Institutional Review Board Committee.
Step 1: systematic literature review and data extraction
To identify relevant studies investigating the association between long-term exposure to ambient PM2.5 and dementia outcomes, we initially scoured PubMed in April 2023, searching for the most recent peer-reviewed systematic review and meta-analysis studies adhering to PRISMA guidelines on long-term PM2.5 exposure and dementia, including both incident dementia and dementia mortality (Supplementary Information). We selected to base our systematic review Wilker et al.13, integrating all the publications they reviewed up to July 2022 into our literature search. Following this, we conducted comprehensive searches across multiple databases (PubMed, Embase and Web of Science) utilizing controlled vocabulary search terms associated with air pollution and dementia (detailed search strings are provided in Supplementary Table 1). This updated literature search aimed to collect newly available epidemiological evidence starting from July 2022, and the search was performed on 15 June 2023. Detailed search terms for each database can be found in the Supplementary Information. We merged the publications from the identified by Wilker et al.13 and the updated search, ultimately selecting 28 (refs. 20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47) studies for our meta-analysis based on our inclusion and exclusion criteria (see below and the Supplementary Information). The systematic review flowchart is depicted in Extended Data Fig. 1.
The systematic review was conducted independently by two reviewers who screened each study for eligibility on the basis of title and abstract. The first reviewer reviewed titles and abstracts of all identified articles. A second investigator reviewed a random sample of 10% of excluded reports for a sensitivity check. The full text of the included studies was retrieved and examined for inclusion in the meta-analysis. Finally, each full-text exclusion was verified by both reviewers. No discrepancy was found.
The searched studies were included if results were based on cohorts or pooled cohorts and reported a quantitative measurement of risk, such as HR, percentage change or β-coefficient associated with a range of PM2.5 exposure change. When multiple studies offered risk estimates from the same cohort, we incorporated only the study with the most extensive sample size or follow-up duration to avoid duplicate data inclusion. In addition, effect estimates had to include a measure of uncertainty for the effect size measure. Exposure levels had to be reported on a continuous scale of PM2.5 values; studies reporting estimates for categorized exposure levels were excluded. Only studies assessing the long-term impact of PM2.5, defined as exposure to annual means, were included. We included study cohorts with an age of 30 years and older at the beginning of the study. While our search was restricted to abstracts in English, we did include studies in all languages (unless translation was not feasible). Finally, studies were included if they assessed the impact of PM2.5 on incidence or mortality outcomes for any of the following types of dementia: all-cause dementia or subtypes of dementia including AD, VaD and senile dementia. We excluded animal studies. A detailed list of inclusion and exclusion criteria is included in the Supplementary Information. The source of all full-text reviewed studies and the corresponding inclusion/exclusion decisions and rationale are presented in Supplementary Table 4.
Data from eligible publications were manually extracted using a standardized template to capture the detailed information of the included studies, such as demographic characteristics, study design, ___location, sample size, duration of follow-up, person-years, effect size, exposure definition, PM2.5 exposure levels (minimum, maximum, mean, s.d., median, 25th and 75th percentiles and interquartile range), measurement methods, outcome definition, ascertainment methods, number of dementia events, risk estimates, associated uncertainties and specific confounders adjusted for in the analysis. To focus on the relationship between PM2.5 exposure and dementia, we extracted effect estimates exclusively from single-pollutant models, without accounting for potential effect modification or interactive effects with other air pollutants. To ensure consistency, we prioritized the most fully adjusted models reported in each study to minimize confounding. We also quantitatively assessed the risk of potential bias for each study, following the GRADE48 and Cochrane76 criteria. Supplementary Table 2 contains a full list of extracted variables.
Step 2: estimate the risk–outcome relationships
We estimated the relationship between ambient PM2.5 and risk of dementia applying the MR-BRT model16. This model allows us to integrate RR estimates from a number of studies across different exposure ranges, and fit a nonlinear relationship between exposure and outcomes with options to impose shape constraints, such as monotonic increasing/decreasing, concave/convex and specific spline settings. In addition, the tool provides a mechanism to account for known differences in study-level characteristics by including and testing potential bias covariates related to study-level characteristics and incorporating into the final model any covariates found to introduce significant bias that would distort effect estimates (see step 3 below). The tool then additionally quantifies remaining unexplained between-study heterogeneity and estimates of uncertainty with and without consideration of this unexplained between-study heterogeneity, which forms the basis from which to calculate the BPRF, ROS and star ratings (see step 6 below). In case of data sparsity, the tool provides the ability to adjust the between-study heterogeneity parameter through a Fisher scoring correction (see step 4 below). Finally, the tool also has the ability to assess publication bias and provides a significance measure (P value < 0.05) (see step 5 below).
We fit curves to the data from all studies and subtype-specific studies. For all types of dementia, we included 49 extracted effect estimates from 28 studies; while for AD, we included 12 and for VaD, 6 extracted effect estimates (Extended Data Fig. 2). The number of studies for other subtypes of dementia was too small to fit individual risk–outcome curves. All exposure-response curves exhibited a harmful effect, meaning the risk of dementia increased with increasing levels of particulate matter pollution. For all curves, we placed three knots at the 25th, 50th and 75th percentile of the exposure distribution. To relax the (log-)linear assumption, our MR-BRT models were designed to flexibly adopt self-defined shape constraints (splines, monotonicity constraint and concavity/convexity constraint), allowing for a more accurate representation of the underlying relationship between PM2.5 and dementia. We fit the final models using a cubic spline with a linear prior on the right tail, along with monotonicity and concavity constraints. Linear-tail constraints are a common way to regularize spline behavior at the outer end of the data range. To make our results robust to knot placement, an ensemble model was created from 50 models using random knot placement by optimizing for model fit (based on a likelihood metric) and total variation (based on the highest derivative). We allowed the model to trim 10% of the data for PM2.5 and all-type dementia as a means to identify outliers and data points increasing between-study heterogeneity. Trimming was not implemented for the subgroup analysis due to limited data points for AD and VaD. Uncertainty estimates for the mean risk curve were generated based on a parametric bootstrapping approach. Further technical details on estimating the risk curve, spline methodology, trimming procedures, the ensemble modeling approach and uncertainty estimation are discussed elsewhere16,18.
We conducted stratified analyses the first of which was based on the method of dementia case diagnosis, using either active ascertainment through physician diagnosis or passive ascertainment through medical records or death certificates, as well as self-reported cases. To better understand air pollution-induced dementia risk among older adults, we conducted an additional stratified analysis focusing on cohorts with a baseline age restriction ≥60 years. Stratified analyses by subregion were also conducted to assess regional variations in the relationship between PM2.5 exposure and dementia. These analyses were limited to studies from North America and Europe, as insufficient data from other regions prevented model convergence.
Sensitivity analyses were further conducted to test the robustness of the model fitting. Sensitivity analysis with no-trimming and 15% trimming for all-type dementia outcomes were implemented to test the potential influence of the outliers. We further evaluated the effects of applying alternative assumptions regarding the monotonic constraint and concavity constraint (Supplementary Information).
Step 3: assess and adjust for biases
In addition to extracting RR estimates, we extracted information regarding study design and other characteristics which could potentially bias the reported effect size. We extracted information based on common sources of bias across six domains as identified through the GRADE criteria48, Cochrane reviews76 and expert suggestions that include representativeness of the study population, exposure, outcome, reverse causation, control for confounding and selection bias. We incorporated 12 study-level covariates into our MR-BRT models, categorized under the six bias domains: (1) study population (4 factors): the representativeness of the study population (0, general population; 1, subgroup population), the method of exposure assessment (0, objective measurement; 1, self-report), restricted to older adults (0, restricted to older adults with baseline age ≥60 years; 1, broader baseline age range, strictly ≥30 but not necessarily ≥60, such as ≥40 or ≥50), geographic ___location (0, North America; 1, Europe; 2, Asia; 3, other regions); (2) exposure (3 factors): the method of exposure assessment (0, objective measurement; 1, self-reported exposure), the spatial resolution of exposure assessment (0, individual-level exposure estimation within a 1 × 1-km area at the individual’s residence; 1, population-level exposure estimation beyond a 1 × 1-km area at the individual’s residence) and the timing of the exposure measurement (0, time-varying exposure; 1, exposure measured only at baseline or at a fixed time point); (3) outcome (2 factors): the specific type of dementia outcome (five binary indicators for AD, VaD, non-AD dementia, senile dementia and other dementia subtype) and the method of outcome assessment (0, based on repeated cognitive testing and physician diagnosis (active ascertainment); 1, based on death certificate, medical record or self-report); (4) reverse causation (1 factor): risk of reverse causation (0, no risk of reverse causation; 1, there is a risk); (5) confounders (1 factor): risk of residual confounding (categorized into three levels: 0, low risk, controlled for age, sex, income, education and smoking; 1, medium risk, controlled for age and sex along with other covariates; and 2, high risk, controlled only for age and sex); and (6) selection bias (1 factor): the follow-up rate (classified into three levels: 0, follow-up rate exceeding 95%; 1, follow-up rate between 85% and 95%; 2, follow-up rate below 85%). See Supplementary Table 2.
We tested the risk of bias through linear regression, defining a gold standard (the preferable study design) (the Supplementary Information contains additional information on covariates extracted). Following a Lasso approach99,100, we ranked all covariates and added selected covariates to the model based on said ranking. Significant covariates remained in the model as the process continued. The selection process was terminated if the last added covariate was not significant. Supplementary Table 6 summarizes our assessment results of the potential bias and study quality for all included studies.
Step 4: quantify between-study heterogeneity and adjust for within-study correlation
Differences in effect estimates across studies are referred to as between-study heterogeneity. They are commonly observed and can be introduced by methodological differences, inconsistencies across different studies, or random variations. Despite their regularity, they might lower trust in study results. After adjusting for selected bias covariates, we accounted for known heterogeneity in input study-level characteristics, but remaining unexplained heterogeneity across studies justifiably reduces trust in findings and therefore should be quantified and reported. To do so, we used a linear mixed-effects model to capture the remaining unexplained between-study heterogeneity by including a study-level random slope with variance quantified by a γ term. We used the Fisher information matrix49 to estimate the uncertainty of the heterogeneity (γ), which is robust to both data sparsity and the presence of within-study correlation. The uncertainty estimations not inclusive of γ reflect conventional estimates of uncertainty; while those that incorporating estimates of between-study heterogeneity quantified by γ can be used to generate the BPRF, ROS and star ratings, which are conservative estimates of the excess health risk associated with exposure to a harmful risk factor and are the primary metrics reported in this study.
Step 5: evaluate risk of publication or reporting bias
Publication bias (the biases or selective publication of studies) is a common concern when conducting meta-analyses. In our framework, we have a twofold approach for assessing publication bias: We visually inspected funnel plots (Figs. 1–3b) displaying the residuals of the risk function and s.d. for asymmetry. In addition, we statistically tested for publication bias using Egger’s regression. Egger’s regression50 is a data-driven approach and is based on the detection of a correlation between the residuals and their s.e. If no publication bias was detected, the process was terminated. If we found evidence of publication of reporting bias, we reported on it but did not incorporate any correction to the risk function. This approach is standard in the general literature.
Step 6: estimate BPRF and compute ROS
We generated the BPRF for PM2.5 and dementia as a combination of the mean effect as reflected by the RR curve and the estimated uncertainty including between-study heterogeneity. The BPRF is defined as the fifth quantile curve, which is the closest to the line of RR equal to 1 (the null) and can be interpreted as the smallest harmful effect at each exposure level. In other words, the BPRF represents the weakest association that is consistent with the available data after accounting for between-study heterogeneity. The larger the difference between BPRF and the null, the stronger the evidence supporting a relationship between exposure and outcome. Subsequently, we calculated the ROS, defined as the signed average log RR of the BPRF over the 15th to 85th percentiles of observed exposures18. A positive ROS suggests evidence of a relationship between the risk (in this study, ambient PM2.5) and the outcome (dementia), with higher ROS values indicating stronger evidence and more consistency in findings. Conversely, negative ROS values indicate a weaker and potentially nonsignificant risk–outcome relationship. To facilitate interpretation and comparison across studies, the BPRF framework translates ROS values into a five-star rating system: ≤0 receives one star; >0.0 to 0.14 receives two stars; >0.14 to 0.41 receives three stars; >0.41 to 0.62 receives four stars; and >0.62 receives five stars. We can interpret the star ratings as a combined measure of effect size and strength of evidence: one star denotes a weak effect and/or lack of consistent evidence across available data, with more stars signifying an increasingly stronger effect and more consistent evidence. Additionally, a zero-star rating is assigned to risk–outcome pairs lacking statistically significant association even when not including between-study heterogeneity (the conventional 95% UI without γ crosses the null). Risk–outcome pairs receiving a 1–5-star rating are considered candidates for inclusion in GBD.
Statistics and reproducibility
Analyses were carried out using R v.4.0.5, Python v.3.8 and Stata v.17. To validate key aspects of the meta-regression model used in this analysis, the following packages were used, as described by Zheng et al.18: metafor (R package available for download at https://www.jstatsoft.org/article/view/v036i03) and dosmesreta (R package available for download at https://www.jstatsoft.org/article/view/v072c01).
This study was a secondary analysis of existing data involving systematic reviews and meta-analyses. No statistical method was used to predetermine sample size. As the study did not involve primary data collection, randomization, blinding and data exclusions are not relevant to this study and, as such, no data were excluded and we performed no randomization or blinding. We have made our data and code available to aid reproducibility.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The findings of this study are based on data extracted from published literature up to June 2023. We conducted systematic literature search in PubMed (https://pubmed.ncbi.nlm.nih.gov), Embase (https://www.embase.com) and Web of Science (https://www.webofscience.com), with detailed search terms provided in the Supplementary Information. We have included the full reference list for all studies incorporated in the systematic review and meta-regression. Supplementary Table 4 presents the full-text reviewed studies, along with the detailed rationale for inclusion or exclusion in the meta-regression. For studies included in the meta-regression, study characteristics and detailed extracted effect sizes are presented (Supplementary Tables 5 and 6 and Extended Data Fig. 2). The template of the data collection form is provided in Supplementary Table 2.
Code availability
Analyses were carried out using R v.4.0.5 and Python v.3.10.9. All code used for these analyses is publicly available online (https://github.com/ihmeuw-msca/burden-of-proof/).
References
Li, J., Han, X., Zhang, X. & Wang, S. Spatiotemporal evolution of global population ageing from 1960 to 2017. BMC Public Health 19, 127 (2019).
GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2100–2132 (2024).
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2133–2161 (2024).
World Health Organization. Risk Reduction of Cognitive Decline and Dementia: WHO Guidelines (WHO, 2019).
Costa, L. G. et al. Effects of air pollution on the nervous system and its possible role in neurodevelopmental and neurodegenerative disorders. Pharmacol. Ther. 210, 107523 (2020).
You, R., Ho, Y.-S. & Chang, R. C.-C. The pathogenic effects of particulate matter on neurodegeneration: a review. J. Biomed. Sci. 29, 15 (2022).
Lee, J. et al. Particulate matter exposure and neurodegenerative diseases: a comprehensive update on toxicity and mechanisms. Ecotoxicol. Environ. Saf. 266, 115565 (2023).
Abolhasani, E. et al. Air Pollution and incidence of dementia: a systematic review and meta-analysis. Neurology 100, e242–e254 (2023).
Ru, M., Brauer, M., Lamarque, J. & Shindell, D. Exploration of the global burden of dementia attributable to PM2.5: What Do we know based on current evidence? GeoHealth 5, e2020GH000356 (2021).
Cheng, S. et al. Long-term particulate matter 2.5 exposure and dementia: a systematic review and meta-analysis. Public Health 212, 33–41 (2022).
Pai, S. J., Carter, T. S., Heald, C. L. & Kroll, J. H. Updated world health organization air quality guidelines highlight the importance of non-anthropogenic PM2.5. Environ. Sci. Technol. Lett. 9, 501–506 (2022).
Livingston, G. et al. Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. Lancet 404, 572–628 (2024).
Wilker, E. H., Osman, M. & Weisskopf, M. G. Ambient air pollution and clinical dementia: systematic review and meta-analysis. BMJ https://doi.org/10.1136/bmj-2022-071620 (2023).
Fu, P. & Yung, K. K. L. Air pollution and Alzheimer’s disease: a systematic review and meta-analysis. J. Alzheimers Dis. 77, 701–714 (2020).
Liu, Q., Cook, N. R., Bergström, A. & Hsieh, C.-C. A two-stage hierarchical regression model for meta-analysis of epidemiologic nonlinear dose–response data. Comput. Stat. Data Anal. 53, 4157–4167 (2009).
Zheng, P., Barber, R., Sorensen, R. J. D., Murray, C. J. L. & Aravkin, A. Y. Trimmed constrained mixed effects models: formulations and algorithms. J. Comput. Graph. Stat. 30, 544–556 (2021).
Burnett, R. T., Spadaro, J. V., Garcia, G. R. & Pope, C. A. Designing health impact functions to assess marginal changes in outdoor fine particulate matter. Environ. Res. 204, 112245 (2022).
Zheng, P. et al. The Burden of Proof studies: assessing the evidence of risk. Nat. Med. 28, 2038–2044 (2022).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ https://doi.org/10.1136/bmj.n71 (2021).
Jung, C.-R., Lin, Y.-T. & Hwang, B.-F. Ozone, particulate matter, and newly diagnosed Alzheimer’s disease: a population-based cohort study in Taiwan. J. Alzheimers Dis. 44, 573–584 (2015).
Chen, H. et al. Exposure to ambient air pollution and the incidence of dementia: a population-based cohort study. Environ. Int. 108, 271–277 (2017).
Carey, I. M. et al. Are noise and air pollution related to the incidence of dementia? A cohort study in London, England. BMJ Open 8, e022404 (2018).
Bowe, B., Xie, Y., Yan, Y. & Al-Aly, Z. Burden of cause-specific mortality associated with PM2.5 air pollution in the United States. JAMA Netw. Open 2, e1915834 (2019).
Grande, G., Ljungman, P. L. S., Eneroth, K., Bellander, T. & Rizzuto, D. Association between cardiovascular disease and long-term exposure to air pollution with the risk of dementia. JAMA Neurol. 77, 801 (2020).
Cerza, F. et al. Long-term exposure to air pollution and hospitalization for dementia in the Rome longitudinal study. Environ. Health 18, 72 (2019).
Ilango, S. D. et al. The role of cardiovascular disease in the relationship between air pollution and incident dementia: a population-based cohort study. Int. J. Epidemiol. 49, 36–44 (2020).
Smargiassi, A. et al. Exposure to ambient air pollutants and the onset of dementia in Québec, Canada. Environ. Res. 190, 109870 (2020).
Ran, J. et al. Long-term exposure to fine particulate matter and dementia incidence: a cohort study in Hong Kong. Environ. Pollut. 271, 116303 (2021).
Yuchi, W., Sbihi, H., Davies, H., Tamburic, L. & Brauer, M. Road proximity, air pollution, noise, green space and neurologic disease incidence: a population-based cohort study. Environ. Health 19, 8 (2020).
Mortamais, M. et al. Long-term exposure to ambient air pollution and risk of dementia: results of the prospective three-city study. Environ. Int. 148, 106376 (2021).
Shaffer, R. M. et al. Fine particulate matter and dementia incidence in the adult changes in thought study. Environ. Health Perspect. 129, 087001 (2021).
Younan, D. et al. Racial/ethnic disparities in Alzheimer’s disease risk: role of exposure to ambient fine particles. J. Gerontol. Ser. A 77, 977–985 (2022).
Sullivan, K. J. et al. Ambient fine particulate matter exposure and incident mild cognitive impairment and dementia. J. Am. Geriatr. Soc. 69, 2185–2194 (2021).
Shi, L. et al. A national cohort study (2000–2018) of long-term air pollution exposure and incident dementia in older adults in the United States. Nat. Commun. 12, 6754 (2021).
Klompmaker, J. O. et al. Effects of exposure to surrounding green, air pollution and traffic noise with non-accidental and cause-specific mortality in the Dutch national cohort. Environ. Health 20, 82 (2021).
Semmens, E. O. et al. Air pollution and dementia in older adults in the Ginkgo Evaluation of Memory Study. Alzheimers Dement. 19, 549–559 (2023).
Wang, X. et al. Association of improved air quality with lower dementia risk in older women. Proc. Natl Acad. Sci. USA 119, e2107833119 (2022).
So, R. et al. Long-term exposure to air pollution and mortality in a Danish nationwide administrative cohort study: Beyond mortality from cardiopulmonary disease and lung cancer. Environ. Int. 164, 107241 (2022).
De Crom, T. O. E. et al. Air pollution and the risk of dementia: the Rotterdam study. J. Alzheimers Dis. 91, 603–613 (2023).
Chen, G.-C., Nyarko Hukportie, D., Wan, Z., Li, F.-R. & Wu, X.-B. The association between exposure to air pollution and dementia incidence: the modifying effect of smoking. J. Gerontol. Ser. A 78, 2309–2317 (2023).
Yang, L. et al. Associations between PM2.5 exposure and Alzheimer’s disease prevalence among elderly in eastern China. Environ. Health 21, 119 (2022).
Wood, D., Evangelopoulos, D., Beevers, S., Kitwiroon, N. & Katsouyanni, K. Exposure to ambient air pollution and the incidence of dementia in the elderly of England: the ELSA cohort. Int. J. Environ. Res. Public. Health 19, 15889 (2022).
Trevenen, M. L. et al. Ambient air pollution and risk of incident dementia in older men living in a region with relatively low concentrations of pollutants: the Health in Men study. Environ. Res. 215, 114349 (2022).
Zhu, Z. et al. Residential greenness, air pollution and incident neurodegenerative disease: a cohort study in China. Sci. Total Environ. 878, 163173 (2023).
Yu, Y. et al. Air pollution and traffic noise interact to affect cognitive health in older Mexican Americans. Environ. Int. 173, 107810 (2023).
Andersson, J. et al. PM2.5 and dementia in a low exposure setting: the influence of odor identification ability and APOE. J. Alzheimers Dis. 92, 679–689 (2023).
Andersen, Z. J. et al. Long-term exposure to air pollution and mortality from dementia, psychiatric disorders, and suicide in a large pooled European cohort: ELAPSE study. Environ. Int. 170, 107581 (2022).
Schünemann, H. et al (eds). GRADE Handbook (2013).
Biggerstaff, B. J. & Tweedie, R. L. Incorporating variability in estimates of heterogeneity in the random effects model in meta-analysis. Stat. Med. 16, 753–768 (1997).
Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. Brit. Med. J. 315, 629–634 (1997).
Cao, Q. et al. The prevalence of dementia: a systematic review and meta-analysis. J. Alzheimers Dis. 73, 1157–1166 (2020).
Goodman, R. A. et al. Prevalence of dementia subtypes in United States Medicare fee‐for‐service beneficiaries, 2011–2013. Alzheimers Dement. 13, 28–37 (2017).
Kuller, L. H. & Ives, D. G. Vital records and dementia. Neuroepidemiology 32, 70–71 (2009).
Gao, L. et al. Accuracy of death certification of dementia in population-based samples of older people: analysis over time. Age Ageing 47, 589–594 (2018).
Emrani, S. et al. Alzheimer’s/vascular spectrum dementia: classification in addition to diagnosis. J. Alzheimers Dis. 73, 63–71 (2020).
Nichols, E. et al. The prevalence, correlation, and co-occurrence of neuropathology in old age: harmonisation of 12 measures across six community-based autopsy studies of dementia. Lancet Healthy Longev. 4, e115–e125 (2023).
Knopman, D. S., Petersen, R. C., Rocca, W. A., Larson, E. B. & Ganguli, M. Passive case‐finding for Alzheimer’s disease and dementia in two US communities. Alzheimers Dement. 7, 53–60 (2011).
Amnuaylojaroen, T. & Parasin, N. Pathogenesis of PM2.5-Related disorders in different age groups: children, adults, and the elderly. Epigenomes 8, 13 (2024).
McDuffie, E. E. et al. Source sector and fuel contributions to ambient PM2.5 and attributable mortality across multiple spatial scales. Nat. Commun. 12, 3594 (2021).
Snider, G. et al. Variation in global chemical composition of PM2.5: emerging results from SPARTAN. Atmospheric Chem. Phys. 16, 9629–9653 (2016).
Russ, T. C., Batty, G. D., Hearnshaw, G. F., Fenton, C. & Starr, J. M. Geographical variation in dementia: systematic review with meta-analysis. Int. J. Epidemiol. 41, 1012–1032 (2012).
Li, W. et al. A review of respirable fine particulate matter (PM2.5)-induced brain damage. Front. Mol. Neurosci. 15, 967174 (2022).
Tian, L. et al. Correlation of regional deposition dosage for inhaled nanoparticles in human and rat olfactory. Part. Fibre Toxicol. 16, 6 (2019).
Burch, W. M. Passage of inhaled particles into the blood circulation in humans. Circulation https://doi.org/10.1161/hc0402.104118 (2002).
Lucchini, R. G., Dorman, D. C., Elder, A. & Veronesi, B. Neurological impacts from inhalation of pollutants and the nose–brain connection. NeuroToxicology 33, 838–841 (2012).
Kritikos, M., Gandy, S. E., Meliker, J. R., Luft, B. J. & Clouston, S. A. P. Acute versus chronic exposures to inhaled particulate matter and neurocognitive dysfunction: pathways to Alzheimer’s disease or a related dementia. J. Alzheimers Dis. 78, 871–886 (2020).
Calderón-Garcidueñas, L., Stommel, E. W., Rajkumar, R. P., Mukherjee, P. S. & Ayala, A. Particulate air pollution and risk of neuropsychiatric outcomes. what we breathe, swallow, and put on our skin matters. Int. J. Environ. Res. Public. Health 18, 11568 (2021).
Calderón-Garcidueñas, L. et al. Environmentally toxic solid nanoparticles in noradrenergic and dopaminergic nuclei and cerebellum of metropolitan Mexico City children and young adults with neural quadruple misfolded protein pathologies and high exposures to nano particulate matter. Toxics 10, 164 (2022).
Kang, Y. J., Tan, H., Lee, C. Y. & Cho, H. An air particulate pollutant induces neuroinflammation and neurodegeneration in human brain models. Adv. Sci. 8, 2101251 (2021).
Peters, A. Ambient air pollution and Alzheimer’s disease: the role of the composition of fine particles. Proc. Natl Acad. Sci. USA 120, e2220028120 (2023).
Brook, R. D. et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the american heart association. Circulation 121, 2331–2378 (2010).
Grande, G. et al. Association of long-term exposure to air pollution and dementia risk: the role of homocysteine, methionine, and cardiovascular burden. Neurology 101, e1231–e1240 (2023).
Saeed, A., Lopez, O., Cohen, A. & Reis, S. E. Cardiovascular disease and Alzheimer’s disease: the heart–brain axis. J. Am. Heart Assoc. 12, e030780 (2023).
Shou, Y. et al. A review of the possible associations between ambient PM2.5 exposures and the development of Alzheimer’s disease. Ecotoxicol. Environ. Saf. 174, 344–352 (2019).
O’Piela, D. R., Durisek, G. R., Escobar, Y.-N. H., Mackos, A. R. & Wold, L. E. Particulate matter and Alzheimer’s disease: an intimate connection. Trends Mol. Med. 28, 770–780 (2022).
Higgins, J. P. T. et al. (eds). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (Cochrane, 2023).
GBD 2021 Risk Factors Collaborators. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2162–2203 (2024).
Institute for Health Metrics and Evaluation. Burden of Proof. https://vizhub.healthdata.org/burden-of-proof/ (2024).
World Health Organization. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. (WHO, 2021).
United States Environmental Protection Agency. National Ambient Air Quality Standards for Particulate Matter (US EPA, 2024).
Australian National Environment Protection Council. National Environment Protection (Ambient Air Quality) Measure. https://www.legislation.gov.au/F2007B01142/latest/text (2021).
Canadian Council of Ministers of the Environment. Canadian Ambient Air Quality Standards. https://www.canada.ca/en/environment-climate-change/services/environmental-indicators/air-quality.html#Methods (2013).
Government of the United Kingdom. The Environmental Targets (Fine Particulate Matter) (England) Regulations 2023. https://www.legislation.gov.uk/uksi/2023/96/contents/made (2023).
European Commission. European Union Air Quality Standards. https://environment.ec.europa.eu/topics/air/air-quality/eu-air-quality-standards_en (2008).
European Commission. Commission welcomes provisional agreement for cleaner air in the EU. https://ec.europa.eu/commission/presscorner/detail/en/ip_24_886 (2024).
Ministry of the Environment Government of Japan. Environmental Quality Standards in Japan. https://www.env.go.jp/en/air/aq/aq.html (2009).
Ministry of Ecology and Environment, the People’s Republic of China. Ambient air quality standards. https://english.mee.gov.cn/Resources/standards/Air_Environment/quality_standard1/201605/t20160511_337502.shtml (2012).
Zheng, P. limetr: linear mixed effects model with trimming. Github https://github.com/zhengp0/limetr (2023).
Zheng, P. xspline: advanced spline tools. GitHub https://github.com/zhengp0/xspline (2024).
Flor, L. S. et al. Health effects associated with exposure to secondhand smoke: a Burden of Proof study. Nat. Med. 30, 149–167 (2024).
Carr, S. et al. A Burden of Proof study on alcohol consumption and ischemic heart disease. Nat. Commun. 15, 4082 (2024).
Gil, G. F. et al. Health effects associated with chewing tobacco: a Burden of Proof study. Nat. Commun. 15, 1082 (2024).
Spencer, C. N. et al. Health effects associated with exposure to intimate partner violence against women and childhood sexual abuse: a Burden of Proof study. Nat. Med. 29, 3243–3258 (2023).
Dai, X. et al. Health effects associated with smoking: a Burden of Proof study. Nat. Med. 28, 2045–2055 (2022).
Razo, C. et al. Effects of elevated systolic blood pressure on ischemic heart disease: a Burden of Proof study. Nat. Med. 28, 2056–2065 (2022).
Lescinsky, H. et al. Health effects associated with consumption of unprocessed red meat: a Burden of Proof study. Nat. Med. 28, 2075–2082 (2022).
Stanaway, J. D. et al. Health effects associated with vegetable consumption: a Burden of Proof study. Nat. Med. 28, 2066–2074 (2022).
Stevens, G. A. et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet 388, e19–e23 (2016).
Efron, B., Hastie, T., Johnstone, I. & Tibshirani, R. Least angle regression. Ann. Stat. 32, 407–489 (2004).
Tibshirani, R. Regression shrinkage and selection via the lasso. J. R. Stat. Soc. Ser. B Methodol. 58, 267–288 (1996).
Acknowledgements
The research reported in this publication was supported by the Bill & Melinda Gates Foundation (OPP1152504). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders. The study funders had no role in study design, data collection, data analysis, data interpretation, writing of the final report or the decision to publish. We thank the Environmental, Occupational and Dietary Risk Factors Team at the Institute for Health Metrics and Evaluation, University of Washington, including S. Spearman, D. Woldegebreal, J. Stanaway and N. Hashmeh, for their valuable input and review of the work.
Author information
Authors and Affiliations
Contributions
M.B., J.S. and K.B. conceived the study. X.H., K.B., M.B., S.I.H. and C.A. managed the estimation or publications process. X.H., K.B. and M.B. wrote the first draft of the paper. A.Y.A., C.J.L.M., P.Z. and R.J.D.S. developed methods or computational machinery. X.H., E.K.M., K.B., M.B. and S.W. had primary responsibility for applying analytical methods to produce estimates. X.H., V.G., J.S.J., F.Y. and S.W. had primary responsibility for seeking, cataloging, extracting or cleaning data, and for designing or coding figures and tables. X.H., K.B., M.B., E.K.M., V.G., J.S.J., F.Y. and J.S. provided data or critical feedback on data sources. X.H., K.B., M.B. and J.S. provided critical feedback on methods or results. X.H., K.B., M.B., J.S., S.A.M., S.I.H. and J.S.J. drafted the work or revised it critically for important intellectual content. X.H., K.B., S.I.H. and C.A. managed the overall research enterprise.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Aging thanks Beate Ritz, Ireneous Soyiri, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 PRISMA flow diagram of PM2.5 exposure and dementia outcomes.
Template is from Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/.
Extended Data Fig. 2 Forest plot of the extracted Hazard Ratios (HR) and corresponding 95% confidence intervals (CI) from all included studies for each dementia outcome, including all-cause dementia (n = 26), Alzheimer’s disease (AD) (n = 12), vascular dementia (VaD) (n = 6), and other types of dementia (n = 5).
The reported HR from the most-adjusted model was extracted for each dementia outcome from each study. If multiple averaging periods were implemented in the same study, the effect estimate using the longest averaging period were extracted and used as input for the meta-analyses. For Bowe 2019, four effect estimates were extracted from nonlinear risk–outcome curve at PM2.5 exposure level of a. 6 μg/m3, b. 10 μg/m3, c. 13 μg/m3, and 16 μg/m3, representing the exposure range of this study. All study-specific effect estimates were scaled to a standard unit change in PM2.5 concentration of 1 μg/m3. Dark green squares represent mean HRs, and light green lines indicate 95% CIs from each study. See Supplementary Table 4 for more details on included observations from each study.
Extended Data Fig. 3 Relationships between PM2.5 exposure and dementia among studies with active ascertainment through physician diagnosis (17 data points from 10 studies).
a, RR function. The solid green line represents the mean RR at each exposure level, and the solid red line represents the Burden of proof risk function. The dark green shaded area indicates the 95% uncertainty interval (UI) without accounting for between-study heterogeneity, while the light green shaded area represents the 95% UI accounting for between-study heterogeneity. The size of the data points is proportional to the inverse of the standard deviation of the effect estimates, where larger points indicate higher precision in the effect estimates. b, A modified funnel plot showing the residuals (relative to zero) on the x axis and the estimated s.d. (inclusive of between-study heterogeneity) on the y axis.
Extended Data Fig. 4 Relationships between PM2.5 exposure and dementia among studies with passive ascertainment through medical records, death certificates, or self-reports (32 data points from 18 studies).
a, RR function. The solid green line represents the mean RR at each exposure level, and the solid red line represents the Burden of proof risk function. The dark green shaded area indicates the 95% uncertainty interval (UI) without accounting for between-study heterogeneity, while the light green shaded area represents the 95% UI accounting for between-study heterogeneity. The size of the data points is proportional to the inverse of the standard deviation of the effect estimates, where larger points indicate higher precision in the effect estimates. b, A modified funnel plot showing the residuals (relative to zero) on the x axis and the estimated s.d. (inclusive of between-study heterogeneity) on the y axis.
Extended Data Fig. 5 Relationships between PM2.5 exposure and dementia among studies restricted to participants aged ≥ 60 years at baseline (28 data points from 15 studies).
a, RR function. The solid green line represents the mean RR at each exposure level, and the solid red line represents the Burden of proof risk function. The dark green shaded area indicates the 95% uncertainty interval (UI) without accounting for between-study heterogeneity, while the light green shaded area represents the 95% UI accounting for between-study heterogeneity. The size of the data points is proportional to the inverse of the standard deviation of the effect estimates, where larger points indicate higher precision in the effect estimates. b, A modified funnel plot showing the residuals (relative to zero) on the x axis and the estimated s.d. (inclusive of between-study heterogeneity) on the y axis.
Extended Data Fig. 6 Relationships between PM2.5 exposure and dementia among studies with a broader baseline age range, not limited to ≥ 60 years (21 data points from 13 studies).
a, RR function. The solid green line represents the mean RR at each exposure level, and the solid red line represents the Burden of proof risk function. The dark green shaded area indicates the 95% uncertainty interval (UI) without accounting for between-study heterogeneity, while the light green shaded area represents the 95% UI accounting for between-study heterogeneity. The size of the data points is proportional to the inverse of the standard deviation of the effect estimates, where larger points indicate higher precision in the effect estimates. b, A modified funnel plot showing the residuals (relative to zero) on the x axis and the estimated s.d. (inclusive of between-study heterogeneity) on the y axis. No trimming was performed to maintain model convergence.
Extended Data Fig. 7 Relationships between PM2.5 exposure and dementia among studies conducted in North America (18 data points from 12 studies).
a, RR function. The solid green line represents the mean RR at each exposure level, and the solid red line represents the Burden of proof risk function. The dark green shaded area indicates the 95% uncertainty interval (UI) without accounting for between-study heterogeneity, while the light green shaded area represents the 95% UI accounting for between-study heterogeneity. The size of the data points is proportional to the inverse of the standard deviation of the effect estimates, where larger points indicate higher precision in the effect estimates. b, A modified funnel plot showing the residuals (relative to zero) on the x axis and the estimated s.d. (inclusive of between-study heterogeneity) on the y axis. No trimming was performed to maintain model convergence.
Extended Data Fig. 8 Relationships between PM2.5 exposure and dementia among studies conducted in Europe (22 data points from 11 studies).
a, RR function. The solid green line represents the mean RR at each exposure level, and the solid red line represents the Burden of proof risk function. The dark green shaded area indicates the 95% uncertainty interval (UI) without accounting for between-study heterogeneity, while the light green shaded area represents the 95% UI accounting for between-study heterogeneity. The size of the data points is proportional to the inverse of the standard deviation of the effect estimates, where larger points indicate higher precision in the effect estimates. b, A modified funnel plot showing the residuals (relative to zero) on the x axis and the estimated s.d. (inclusive of between-study heterogeneity) on the y axis. No trimming was performed to maintain model convergence.
Supplementary information
Supplementary Information
Supplementary Methods, Figs. 1–3 and Tables 1–12.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, X., Steinmetz, J., Marsh, E.K. et al. A systematic review with a Burden of Proof meta-analysis of health effects of long-term ambient fine particulate matter (PM2.5) exposure on dementia. Nat Aging 5, 897–908 (2025). https://doi.org/10.1038/s43587-025-00844-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-025-00844-y