Abstract
Infection is a devastating post-surgical complication, often requiring additional procedures and prolonged antibiotic therapy. This is especially relevant for craniotomy and prosthetic joint infections (PJI), both of which are characterized by biofilm formation on the bone or implant surface, respectively, with S. aureus representing a primary cause. The local tissue microenvironment likely has profound effects on immune attributes that can influence treatment efficacy, which becomes critical to consider when developing therapeutics for biofilm infections. However, the extent to which distinct tissue niches influence immune function during biofilm development remains relatively unknown. To address this, we compare the metabolomic, transcriptomic, and functional attributes of leukocytes in mouse models of S. aureus craniotomy and PJI complemented with patient samples from both infection modalities, which reveals profound tissue niche-dependent differences in nucleic acid, amino acid, and lipid metabolism with links to immune modulation. These signatures are both spatially and temporally distinct, differing not only between infection sites but evolving over time within a single model. Collectively, this demonstrates that biofilms elicit unique immune and metabolic responses that are heavily influenced by the local tissue microenvironment, which will likely have important implications when designing therapeutic approaches targeting these infections.
Similar content being viewed by others
Introduction
Surgical site infections (SSIs) are among the most devastating complications following invasive procedures. The risk of SSI is influenced by surgical complexity, patient comorbidities, and geographical and anatomical ___location and is reported to occur in 1.6–3.7% of all surgeries1, but may exceed 15% in some cases2,3,4. Staphylococcus aureus (S. aureus) is a leading cause of SSI5 due to a high rate of asymptomatic colonization in the general population (~30%)6 and its ability to infect most human tissues7. Our laboratory studies host-pathogen interactions between S. aureus and the immune system in the setting of two SSIs that progress to biofilm formation, namely craniotomy8 and prosthetic joint infection (PJI)9.
Craniotomy involves the surgical excision of bone from the skull (i.e., bone flap), allowing access to the intracranial compartment for several indications, including resection of brain tumors and epileptic foci or evacuation of traumatic intracranial hemorrhage. Infection occurs when a pathogen, most commonly S. aureus10,11 (~50% of cases), colonizes the bone flap surface and invades the surrounding brain and extracranial tissue. S. aureus, and other pathogens, form a biofilm on the bone flap, which contains metabolically dormant bacterial subpopulations, conferring antibiotic and immune tolerance to the pathogen7,10 and permitting chronic infection9,12. Using a mouse model of S. aureus craniotomy infection, our laboratory has shown that the immune response is compartmentalized, with neutrophil (PMN) and granulocytic myeloid-derived suppressor cell (G-MDSC) infiltrates dominating the bone flap and subcutaneous galea surrounding the biofilm13,14,15. G-MDSCs are pathologically activated PMNs that possess immunosuppressive properties by their ability to inhibit T cell proliferation9 and PMN antimicrobial activity16 along with robust IL-10 production13,17. PMNs and G-MDSCs are also recruited to the brain parenchyma during craniotomy infection; however, they are less abundant compared to monocyte infiltrates. The influx of adaptive immune cells is unique to the brain, along with contributions from brain-resident microglia and astrocytes11,13,14,15.
Arthroplasties can also be complicated by SSI occurring at a frequency of 1–3%, many of which are caused by S. aureus (~30% of cases)18,19,20,21 that forms a biofilm on the implant surface9,22,23. Using a mouse model of PJI, we have shown that G-MDSCs are the most abundant leukocyte infiltrate, followed by PMNs and few monocytes/macrophages17,24,25, broadly resembling the cellular composition in the galea during craniotomy infection13,14,15. Despite these similarities in granulocyte recruitment, depletion of Ly6G+ cells (i.e., G-MDSCs and PMNs) in each model leads to opposite outcomes. Namely, anti-Ly6G enhances S. aureus outgrowth during craniotomy infection but reduces bacterial burden during PJI17,23,24, which is likely driven by the increased abundance of anti-inflammatory G-MDSCs in PJI compared to craniotomy infection9,26.
Current medical management of both craniotomy and PJI requires additional surgeries to remove the biofilm nidus (i.e., bone flap or infected hardware, respectively) along with prolonged antibiotic therapy27,28. Despite this regimen, treatment failure and reinfection rates are appreciably high (10–25%)27,29,30,31, and the inability to resolve infection results in significant morbidity (up to 5–18%) and mortality11,28,32,33. When considering current pathogen-focused treatment strategies28,34, rising antimicrobial resistance35, and paucity of host-directed therapeutic options, there is a need to develop immune-targeted approaches that may, in combination with antibiotics, resolve infection without the need for additional surgeries. This possibility will rely on advances in our understanding of how biofilm formation circumvents immune-mediated clearance. This immune-evasive ability is underscored by repeated failures to develop an S. aureus vaccine despite upwards of 30 clinical trials being conducted36,37,38,39. Undoubtedly, much of the difficulty in this approach lies in the ability of S. aureus to produce numerous virulence factors that target both innate and adaptive immunity, such as mechanisms to evade Toll-like receptor 2 signaling40,41 as well as superantigens42 and protein A43. However, the ability of S. aureus to infect nearly every tissue in the human body44 will likely add additional complexity to antimicrobial efforts, as distinct tissue niches may result in alternative immune cell programming. In recent years, there has been great interest in how the tissue microenvironment influences immune responses during infection45,46,47; however, a direct comparison of how immune function is altered in distinct tissue niches during biofilm infection has not yet been investigated. Such information may identify unique and shared immune characteristics that could be leveraged for therapeutic benefit. The objective of this study was to identify metabolic, transcriptional, and functional differences in the immune response across distinct biofilm niches (craniotomy and PJI) caused by the same pathogen (S. aureus) over time and across tissue locations, and how these changes may promote chronic infection.
Here we report that the local tissue microenvironment elicits unique immune responses during S. aureus craniotomy and PJI, identifying spatial and temporal differences in immune infiltrates and cytokine/chemokine production both within and between these biofilm infections. Metabolic profiling using liquid chromatography-high resolution mass spectrometry (LC–HRMS) identified distinct metabolic signatures in granulocytes that were unique to each tissue niche, representing fatty acid metabolism, amino acids, and nucleic acids. These changes were corroborated by divergent transcriptional profiles of granulocytes recovered from each infection model. Single-cell transcriptomics of patients with craniotomy or PJI also revealed niche-specific transcriptional signatures, reinforcing observations from the mouse models. Our data demonstrate that biofilm infections are characterized by profound metabolic heterogeneity, both within tissues and granulocyte infiltrates, that is influenced by the local microenvironment. This will be important to consider when developing immune-based therapies to avoid dependence on factors that may differ across time and infectious niches.
Results
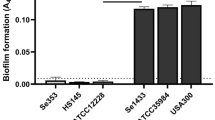
The immune response to biofilm is characterized by temporal and spatial heterogeneity
Our laboratory has extensively utilized mouse models of S. aureus craniotomy10,12,13,14,15,48 and PJI17,24,25 that share many characteristics, including a low infectious inoculum (103 CFU), biofilm morphology8,9, presence of G-MDSC infiltrates, and infection chronicity12,13,15,17. Although we have independently identified unique immune features in each model over the years, suggesting an important contribution of tissue niche in shaping immune responses, a comprehensive and direct comparison between the two has not yet been performed. Therefore, the heterogeneity between infection sites was explored focusing on immune and metabolic profiles over a 2-week interval (Fig. 1A). Comparisons with sham (non-infected) or healthy tissues were not performed due to minimal immune infiltrates following craniotomy (Supplementary Fig. 1) or arthroplasty in the absence of infection24 and the lack of granulocytes in healthy tissues, which was a major cell population of interest in this report. Therefore, assessments between infected tissues across time and ___location were used throughout this study. In general, bacterial burden in both models gradually declined over time, being more widespread in PJI samples and largely restricted to the brain during craniotomy infection (Fig. 1B, C). Significant increases in the absolute numbers of leukocyte populations and total CD45+ cells were observed during PJI between days 3 and 7 or 14 post-infection (Supplementary Fig. 2A, B), coinciding with reduced bacterial abundance at these later intervals (Fig. 1B), whereas changes in immune composition were not as pronounced (Fig. 1D). During craniotomy infection, the most dramatic temporal shifts in immune populations were observed in the brain on days 7 and 14 (Fig. 1D), which corresponded with reduced bacterial burden in this compartment (Fig. 1C). Specifically, CD4+ and γδ T cell infiltrates and activated microglia (CD45lowCX3CR1+MHCII+) were significantly higher at days 7 and 14 post-infection (Fig. 1D), with similar trends in absolute cell counts (Supplementary Fig. 2A). In the galea, only a small increase in CD45+ cells was evident at day 7 post-infection (Supplementary Fig. 2C), which coincided with reduced bacterial burden in this tissue niche (Fig. 1C).
A Overview of experimental models where B–F mice were subjected to either craniotomy (red; n = 20 animals for all groups) or PJI (blue; day 3, n = 12; day 7, n = 13; day 14, n = 14) and sacrificed at the indicated time points, whereupon specimens were collected and assessed for B, C bacterial burden, D immune populations, and E, F intracellular cytokine staining. Data pooled from three independent experiments reported as mean ± SEM. Two-way ANOVA with Tukey’s multiple comparison test. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. Schematic in (A) created in BioRender. BioRender.com/l60v600. Source data are provided as a Source Data file.
The activation status of various immune populations was next assessed by intracellular cytokine staining, revealing both similarities and differences between cell types and within the same leukocyte subset across infection models. All cellular infiltrates during PJI displayed significant decreases in TNF, IL-1β, and IL-6 production as infection progressed, which was generally similar to craniotomy-associated monocytes and macrophages (Fig. 1E). However, granulocytes infiltrating craniotomy infection diverged from their PJI counterparts, with significant increases in IL-10 and IL-1β production over time in G-MDSCs and PMNs, respectively, with IL-1β also elevated in G-MDSCs in the galea at day 14 (Fig. 1E). In the brain, γδ T cells were most active at day 3 post-infection, and activated microglia displayed a spike in TNF and IL-1β but not IL-10 production at day 7 post-infection (Fig. 1F), aligning with the increased abundance of activated microglia (Fig. 1D) and decreased bacterial burden in the brain at day 7 (Fig. 1C).
We next examined inflammatory mediator production in tissue homogenates from PJI and craniotomy infection. Despite cell type- and model-specific increases in some cytokines at the cellular level (Fig. 1E, F), cytokine (Fig. 2A–F), chemokine (Fig. 2G–K), and growth factor (Fig. 2L) concentrations in tissue homogenates largely decreased over time (Supplementary Fig. 2D), with notable exceptions being IL-17, CXCL10, and CCL5 that peaked at day 7 in both infection models (Fig. 2E, H, and K, respectively). Overall, these data indicate that the brain niche elicits unique immune infiltrate and cytokine production profiles compared to the infected galea and bone flap as well as PJI tissue, where these measures remained relatively constant over time.
Supernatants collected from craniotomy (brain and galea; red; n = 15 animals/group) and PJI (joint and soft tissue surrounding the knee; blue; days 3 and 7, n = 13; day 14, n = 14) homogenates were assayed for cytokine (A–F), chemokine (G–K), and growth factor (L) content using a MILLIPLEX MAP 25-plex assay with data normalized to protein content. Data pooled from three independent experiments and represent mean ± SEM. A–L Mixed-effects model with Geisser–Greenhouse correction and Tukey’s multiple comparison test. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. Source data are provided as a Source Data file.
Craniotomy and PJI microenvironments are metabolically diverse
Since unique immune signatures were apparent between craniotomy and PJI and metabolite availability has been shown to modulate immune function49,50,51,52,53,54,55,56,57,58,59, including during PJI17,25,60, we next determined if metabolic diversity also occurred at the tissue level by quantifying extracellular metabolites in homogenates from craniotomy (galea and brain) and the soft tissue surrounding the infected joint (referred to as PJI tissue throughout the manuscript) by LC–HRMS (Fig. 3A). Principle component analysis (PCA) revealed that the brain tissue metabolome was highly divergent from galea and PJI tissue samples at all time points assessed (Fig. 3B). The vast majority of the 226 identified metabolites were significantly altered in at least one comparison, either temporally or spatially, further emphasizing the metabolic diversity between infected tissue sites (Fig. 3C).
A Schematic of metabolomics workflow where mice were subjected to craniotomy or PJI and sacrificed at days 3, 7, and 14 post-infection, whereupon metabolites were isolated from homogenates prepared from galea and PJI tissues and analyzed using LC–HRMS (n = 15 mice/infection model/time point of which three animals were pooled, resulting in five biological replicates per time point). B PCA and C one-way ANOVA p-value analysis of detected metabolites across samples were used to illustrate metabolic heterogeneity between groups and D percentage of significantly altered metabolites among all detected chemical species for each time point. E–G Metabolite differences between models are presented as heat maps of log-transformed normalized peak intensities and H–J PCA plots of comparisons analyzed. (D–G) Data analyzed by MetaboAnalyst with two-sided t-test. Only significant comparisons are shown (p < 0.05). Schematic in (A) created in BioRender. BioRender.com/l13z367. Source data are provided as a Source Data file.
To assess the metabolic profiles of each biofilm infection site on a global scale, metabolites from all time points and samples within each model were bioinformatically pooled. We found that ~75% of detected metabolites were altered between the brain vs. galea or PJI tissue, with 36% of metabolites diverging between galea and PJI tissue (Supplementary Fig. 3A, B). Ingenuity pathway analysis (IPA) revealed that metabolites from brain samples were significantly enriched in multiple pathways relative to both galea (Supplementary Fig. 3C) and PJI tissue (Supplementary Fig. 3D), including histidine catabolism, glutamate and glutamine metabolism, mitochondrial biogenesis, aspartate and asparagine metabolism, and tRNA charging (Supplementary Fig. 3C, D). Galea and PJI tissues also shared significantly enriched pathways relative to the brain, including nucleotide catabolism and transport of bile salts and organic acids, metal ions, and amine compounds (Supplementary Fig. 3C, D). Timepoint agnostic comparisons between galea and PJI samples revealed only PJI-specific enrichments in nucleotide salvage (Supplementary Fig. 3E).
Given the large disparities between brain and galea/PJI metabolomes (Fig. 3B), further comparisons were limited to galea vs. PJI tissue based on similarities in bacterial burdens (Fig. 1B, C) and granulocyte infiltrates (Fig. 1D). A total of 33–70% of detected metabolites were differentially present in galea vs. PJI tissue, depending on time point (Fig. 3D). At day 3 post-infection, clear distinctions in nucleotide metabolites were evident, where UMP, AMP, thymine, and cytosine were increased in the galea, while uridine, adenosine, and adenine were enriched in PJI tissue (Fig. 3E). Amino acid levels were also differentially detected, with valine, methionine sulfoxide, and acetylhistamine increased in galea, whereas glutamate, glutamine, and dimethyl-L-arginine were elevated in PJI. Divergences in nucleotide and amino acid species between craniotomy and PJI persisted at day 7 (Fig. 3F); however, the specific metabolites affected were largely distinct from those observed at day 3. In contrast, only 33% of metabolites differed between galea and PJI tissue at day 14 post-infection (Fig. 3D); however, several nucleotides and amino acids were still differentially enriched in the galea, including UMP, AMP, and asparagine, as well as multiple dipeptide species (Fig. 3G). PCA highlighted the distinct extracellular metabolomes between galea and PJI tissues at all time points (Fig. 3H–J). Pathway analysis confirmed the importance of nucleotide and amino acid metabolism, with nucleotide salvage and catabolism metabolites exhibiting a PJI bias at day 3, which shifted to galea at later time points (Supplementary Fig. 4A–C). Similarly, glutamate/glutamine and aspartate/asparagine metabolism pathways were more prominent in PJI tissues at day 3 (Supplementary Fig. 4A), which transitioned to higher abundance in the galea at days 7 and 14 post-infection (Supplementary Fig. 4B, C).
Finally, a kinetic analysis was performed to assess the evolution of extracellular tissue metabolomes over time within a single compartment. Temporal changes in metabolites were most apparent in PJI tissue, with 63% of detected species differing across time points (Fig. 4C), compared to 13% and 27% of brain and galea metabolites, respectively (Fig. 4A, B). Brain and galea metabolites clustered distinctly at all time points by PCA across PC2 but not PC1 (Fig. 4D, E), whereas PJI tissues were indistinguishable at days 7 and 14 by PCA but distinct from day 3 samples (Fig. 4F). When examined in greater detail, infected brain and galea samples displayed unique metabolic signatures at each interval (Fig. 4G, H), whereas the majority of differentially expressed metabolites in PJI tissue occurred between days 3 and 7 and remained largely unchanged at day 14 post-infection (Fig. 4I), in agreement with PCA (Fig. 4D–F). Notably, as infection progressed in the brain, amino acids such as aspartic acid, valine, proline, and histidine increased in abundance (Fig. 4G). Similar elevations in aspartic acid and asparagine were observed in the galea at day 7 post-infection, which waned by day 14 (Fig. 4H). UMP and AMP levels were highest at day 3 post-infection in the galea, whereas various nitrogenous bases (hypoxanthine, uridine, xanthine, thymine, cytosine) were enriched at later time points (Fig. 4H). In PJI tissues, valine derivatives, aspartic acid, and glutamine were detected at later time points, along with aconitic acid (Fig. 4I). These results reveal considerable spatial and temporal shifts in extracellular tissue metabolites during craniotomy and PJI, gradually evolving over time in the brain and galea but with an abrupt transition between days 3 and 7 post-infection in PJI tissue. Furthermore, this demonstrates that PJI tissue and galea niches, while more alike compared to the brain, are nonetheless distinct, especially in metabolites associated with nucleotide metabolism/salvage and various amino acids, which may influence the observed differences in the immune response across time and ___location.
The dataset from Fig. 3 was reanalyzed to assess temporal changes within each infection site over time. A–C The percentage of significantly altered extracellular metabolites among all detected chemical species across time within each niche and D–F PCA was used to illustrate metabolic heterogeneity between time points within infection sites. G–I Metabolites changed over time are presented as heat maps of log-transformed normalized peak intensities. Data analyzed by MetaboAnalyst using one-way ANOVA and only significant comparisons are shown (p < 0.05). Source data are provided as a Source Data file.
Granulocytes display temporal and spatial metabolic heterogeneity during biofilm infection
Given the observed metabolome differences between tissue niches (Fig. 3) and that metabolism influences leukocyte effector functions17,56,58,61, we next compared the intracellular metabolome of Ly6G+ granulocytes, the most prominent leukocyte infiltrate in galea and PJI tissues, using LC–HRMS (Fig. 3A). This approach revealed significant heterogeneity, with 12–63% of detected granulocyte metabolites differing between biofilm models, depending on time point (Fig. 5A). These differences were most apparent at days 3 and 14 by PCA, with overlap between galea and PJI granulocyte metabolomes occurring at day 7 post-infection (Fig. 5B). Nevertheless, significantly altered metabolites between granulocytes from both biofilm models were detected at all time points (Fig. 5C–E). Similar to extracellular metabolite analysis, temporal changes in the granulocyte metabolome were also investigated in each tissue niche. Granulocytes recovered from craniotomy infection exhibited substantial metabolic shifts, with many amino acids significantly elevated at days 3 and 7 that transitioned to a small number of fatty acids by day 14 post-infection (Fig. 5H). This was supported by PCA, where all three time points clustered separately (Fig. 5F). In contrast, granulocytes isolated from PJI tissue showed few metabolic changes over time, with only myristic and citric acid significantly elevated at day 3 relative to days 7 and 14 post-infection (Fig. 5I). Again, this was reflected by PCA where all three time points displayed a high degree of overlap (Fig. 5G). These results establish that the metabolomes of granulocytes infiltrating different biofilm niches are distinct, with greater temporal diversity in craniotomy than PJI, the latter of which remained largely metabolically static. These changes, in addition to extracellular tissue metabolome shifts, may partially explain the observed alterations in functional immune profiles (Fig. 1E).
Mice subjected to craniotomy or PJI were sacrificed at days 3, 7, and 14 post-infection, whereupon Ly6G+ granulocytes were recovered from galea and PJI tissue. Intracellular metabolites were extracted from cells and analyzed by LC–HRMS (n = 15 mice/infection model/time point of which three animals were pooled, resulting in five biological replicates per time point). A Percentage of significantly altered metabolites among all detected chemical species and B PCA plots for each time point are shown. Craniotomy and PJI samples were assessed for metabolic changes longitudinally (H, I) as well as by time point across models (C–E) and presented as a heat map of log-transformed normalized peak intensities. F, G PCA plots of longitudinal analyses are also presented. Data analyzed by MetaboAnalyst with (H, I) one-way ANOVA or (A, C–E) two-tailed t-test. Only significant comparisons are shown (p < 0.05). Source data are provided as a Source Data file.
Metabolomic enrichment analysis reveals key temporal and spatial changes in pathway flux
Given the extensive metabolic differences across biofilm infection models and time, quantitative enrichment analysis (QEA) was performed using the MetaboAnalyst platform62 to identify biologically meaningful pathways. Analysis was conducted using human metabolomic database (HMDB) identifiers63 and the KEGG suite of metabolic pathways64. QEA of extracellular metabolomic differences between craniotomy and PJI microenvironments confirmed the overabundance of nucleic acid changes, with pyrimidine and purine metabolism identified as enriched pathways at each time point assessed (Fig. 6A), in agreement with IPA (Supplementary Fig. 4A–C) and metabolite level analysis (Fig. 3E–G). Time series evaluation revealed that pyrimidine metabolites were also significantly enriched over time in the brain and galea but not in PJI (Fig. 6B). Interestingly, similar increases in intracellular purine and pyrimidine metabolites were observed in granulocytes across models at day 14 but failed to reach significance at days 3 or 7 post-infection (Fig. 6C), and intracellular purines differed over time, specifically in granulocytes from the galea but not PJI tissue (Fig. 6D). Across granulocytes isolated from craniotomy and PJI, the most striking difference in intracellular metabolites concerned pathways of lipid and fatty acid metabolism at days 3 and 14 post-infection (Fig. 6C).
Quantitative enrichment analysis for both extracellular tissue (A, B) and granulocyte (C, D) metabolomic comparisons performed in Figs. 3, 4, and 5 are shown. Enrichment ratios were calculated by the number of significantly differentially detected metabolites as a fraction of total pathway constituents. Craniotomy vs. PJI comparisons (A, C) were conducted using categorical/classification grouping, while timeseries comparisons (B, D) were analyzed by continuous regression. A–D Data analyzed with MetaboAnalyst Enrichment tests based on well-established globaltest116 methodology. Significant pathways are shown in graded colors (p < 0.05), whereas non-significant pathways are depicted in gray and fall left of the significance line. Source data are provided as a Source Data file.
This analysis also confirmed the importance of shifts in various amino acid species observed both extracellularly in tissues (Figs. 3 and 4) and within granulocytes (Fig. 5). Alanine, aspartate, and glutamine were differentially abundant in extracellular tissue samples at all intervals (Fig. 6A) as well as across time in the brain (Fig. 6B) and within granulocytes in the galea (Fig. 6D). Pathways of tryptophan metabolism were also identified in extracellular tissue (Fig. 6A, B), but not in granulocytes. Histidine metabolism was altered in the brain microenvironment (Fig. 6B), confirming IPA results (Supplementary Fig. 3C, D). Finally, arginine pathways, a metabolite linked to G-MDSC immunosuppressive function16, were significantly enriched in extracellular tissues across models at later time points (days 7 and 14; Fig. 6A) as well as over time specifically within granulocytes from the galea (Fig. 6D). These pathway analyses validate our observations of spatial and temporal differences in nucleotide, fatty acid, and amino acid levels during biofilm infection as well as provide specific targets for future exploration to evaluate impact on the immune response.
Granulocytes exhibit divergent transcriptional programs during prosthetic joint and craniotomy infection
Since our findings identified differences in granulocyte inflammatory activity (Fig. 1E) and intracellular metabolomes (Fig. 5C–E) during craniotomy and PJI, we postulated that granulocytes may exhibit altered transcriptional states in these unique tissue niches, potentially underlying observed functional differences. Therefore, we next compared the transcriptional signatures of Ly6G+ granulocytes in galea vs. PJI tissue using bulk RNA-seq. This comparison was valid since both shared similar attributes in terms of bacterial abundance (Fig. 1B, C), predominance of G-MDSC and PMN infiltrates (Fig. 1D), and proximity to the biofilm nidus on the implant or bone flap surface. Distinct transcriptional profiles were observed between Ly6G+ granulocytes recovered from the two niches (Fig. 7A), with 1870 genes significantly upregulated during craniotomy infection and only 74 increased during PJI (Fig. 7B). Using IPA, the top differentially expressed pathways characterizing PJI granulocytes involved aspects of interferon signaling (Fig. 7C), with the top 3 upregulated molecules belonging to the interferon-induced protein with tetratricopeptide repeats (IFIT) family (Fig. 7D). Gene set enrichment analysis (GSEA) independently validated the impact of tissue niche on granulocyte IFN expression, where the cellular response to IFN-β pathway was significantly increased in PJI relative to craniotomy infection (Fig. 7F). Other notable pathways in PJI-associated granulocytes included PD-1/PD-L1 cancer immunotherapy and PPARα/RXRα activation (Fig. 7C), both previously implicated in G-MDSC function65,66. Granulocytes infiltrating craniotomy infection were enriched in signaling pathways for neuroinflammation, mTOR, eIF2, macrophage alternative activation, IL-10, and unfolded protein response (Fig. 7C). Granulocytes from craniotomy infection also displayed significant increases in organic acid transport (Fig. 7E) and response to fatty acid (Fig. 7G), pathways related to metabolic fluxes identified in our enrichment analyses (Fig. 6C). Since G-MDSCs are pathologically activated PMNs and both cell types were present in each tissue milieu (Fig. 1D), we used a G-MDSC gene set67 to bioinformatically demonstrate an enhanced G-MDSC-like signature in granulocytes isolated from PJI relative to craniotomy infection (Fig. 7H). Conversely, greater PMN-like transcriptional profiles were observed in granulocytes infiltrating craniotomy infection compared to PJI (Fig. 7H). Collectively, these findings demonstrate that granulocyte transcriptional programs are strongly influenced by signals unique to distinct tissue niches despite sharing biofilm attributes8,9.
Mice subjected to craniotomy or PJI (n = 9 mice/model) were sacrificed at day 7 post-infection, whereupon Ly6G+ granulocytes were recovered from the galea and PJI tissue. Cells were pooled from three animals per model, resulting in three biological replicates. RNA was extracted and analyzed by bulk RNA-seq. A PCA and B volcano plots were used to illustrate transcriptional heterogeneity between groups and IPA was used to generate C pathway and D molecular analysis of differentially expressed genes. Independently, E–G gene set enrichment analysis (GSEA) was also conducted and presented as a heat map of sample normalized gene counts. H A published gene set was used to identify G-MDSC or PMN-transcriptional biases and statistical differences were determined between models with a two-tailed Student’s t-test (mean ± SEM; *p = 0.0365, **p = 0.0091). B DESeq2 was used to determine differential gene expression with control for false discovery rate. C–D A statistical pipeline in IPA was used to identify significant pathway and molecule differences, which relies on the right-tailed Fisher’s Exact Test. Source data are provided as a Source Data file.
The human immune response during craniotomy and PJI is transcriptionally diverse
To examine whether leukocyte responses are influenced by biofilm niche during human infection, we compared prior scRNA-seq datasets from patients with craniotomy infection (n = 4) and PJI (n = 3) (Table 1). This analysis included cells recovered from residual surgical samples of galea, bone flap, and intracranial tissue (craniotomy) as well as PJI tissue along with blood leukocytes from each patient as a comparator, resulting in 19 samples and a total of 106,392 high-quality single-cell transcriptomes. Each cell was bioinformatically assigned an identity using the Human Primary Cell Atlas68 and the SingleR package69 before integration and uniform manifold approximation and projection (UMAP) visualization (Fig. 8A). The predominant cell type identified was PMNs, followed by T cells and monocytes, with minor representation of other immune populations (Fig. 8B). Of note, PMNs in this dataset reflect a heterogeneous mix of PMNs and G-MDSCs since the Human Primary Cell Atlas does not have the resolution to distinguish G-MDSCs from PMNs68. This best modeled our transcriptional studies in mouse biofilm models that were also performed with total granulocytes (PMNs and G-MDSCs; Fig. 7). Stratification of UMAP by infection ___location revealed cells with both divergent and similar transcriptomes between infectious niches. For example, some PMNs clustered nearly entirely by craniotomy or PJI origin, whereas others were shared between both infections (Fig. 8G). Nevertheless, PMNs, T cells, and monocytes were all represented in each infection type (Fig. 8C, D). Cells also clustered distinctly based on specimen source (Fig. 8E, F), highlighting that the local tissue milieu influences transcriptional heterogeneity during human biofilm infection.
Single cells from blood and tissue samples of three PJI and four craniotomy infection (Cranio) patients were analyzed by scRNA-seq. A, B Cell identity separated by C, D infection type and E, F specimen source was overlayed on the integrated UMAPs (A, C, E) and (B, D, F) summarized in aggregate to describe the dataset. G PMNs were segmented from the larger dataset, H assessed for infection site composition, and I galea and PJI tissue PMNs were differentially analyzed by IPA to identify pathways enriched in each tissue milieu. A statistical pipeline in IPA was used to identify significant pathway differences, which relies on the right-tailed Fisher’s exact test. HSC hematopoietic stem cell. Source data are provided as a Source Data file.
Further interrogation of this dataset was performed by differential analysis for the three most abundant cell types (PMNs, T cells, and monocytes; Fig. 8B) in PJI tissue vs. galea (craniotomy), which is supported by each population having substantial representation across tissue milieus (Fig. 8F) and subjects (Fig. 8D). Total PMNs segmented from the parent dataset were broadly distributed by sample origin (Fig. 8G, H), and differentially expressed genes between PMN clusters in infected galea vs. PJI tissue were analyzed by IPA. Oxidative phosphorylation and electron transport chain pathways were significantly enriched in PJI, whereas protein production and signaling, as well as ion channel transport pathways, were associated with galea PMNs (Fig. 8I). Interestingly, a few significantly enriched pathways were conserved between human PJI tissues and the mouse PJI model, including PPAR signaling and PD-1/PD-L1 (Figs. 8I and 7C, respectively). Likewise, pathways in galea tissues from human craniotomy infection were also detected in the mouse craniotomy model, including eIF2 and neuroinflammation signaling (Figs. 8I and 7C, respectively). Several amino acid metabolism pathways were significantly enriched in PMNs from human craniotomy tissue relative to PJI (Fig. 8I), and it was interesting that various amino acids were significantly decreased in PMNs infiltrating the infected galea relative to PJI in our mouse studies (Fig. 5E). This suggests that amino acid metabolism may become selectively disrupted within the galea infectious milieu, which was supported by our metabolic enrichment analyses (Fig. 6C, D).
Human T cells were most abundant in blood (Supplementary Fig. 5A, B); however, appreciable T cell numbers were obtained from galea and PJI tissues to allow for differential analysis, which revealed enrichment in PPAR signaling and PD-1/PD-L1 pathways in PJI tissue (Supplementary Fig. 5C), in agreement with the PMN results (Fig. 8I). In contrast, T cells infiltrating infected galea were associated with increased MHC Class I processing/presentation, serotonin and glutaminergic receptor signaling, and senescence pathways. Human monocytes (Supplementary Fig. 5D) were sparse in galea and PJI tissues compared to the blood (Supplementary Fig. 5E), agreeing with our mouse models (Fig. 1D). Pathway analysis revealed similar patterns to T cells and PMNs, with PPAR and oxidative phosphorylation pathways elevated in monocytes from human PJI tissue, whereas insulin and glutaminergic receptor signaling pathways were elevated in the infected galea (craniotomy) (Supplementary Fig. 5F). Collectively, these findings reveal that the transcriptional programs of human leukocytes are influenced by the local tissue milieu during biofilm infection and exhibit striking similarities across cellular lineages.
Discussion
Immune responses are context-dependent and influenced by microenvironmental factors45,70,71,72,73. Despite this knowledge, there is little information on how tissue niches influence immune reactivity in the setting of S. aureus biofilm infection. We addressed this question using two mouse biofilm infection models that share similar features in terms of bacterial burden and predominance of granulocyte infiltrates8,9,11,26. Although both are typified by biofilm formation, craniotomy and PJI models displayed profound differences in intra- and extracellular metabolites, transcriptional programs, and leukocyte activation that were temporally and spatially distinct. Importantly, transcriptional heterogeneity across PJI and craniotomy infections was also observed in patient samples using single-cell transcriptomics. Collectively, these findings reveal a complex picture of how the immune response is shaped by an evolving microenvironment in vivo.
Examination of metabolic profiles in the mouse PJI model, both at the tissue level and in granulocytes, revealed a bimodal pattern with a distinct shift in metabolite composition between days 3 and 7 post-infection. This timing coincides with S. aureus biofilm formation, which is known to occur by day 7 post-infection, as reflected by scanning electron microscopy9 or antibiotic tolerance25. Leukocyte activation was also altered at this interval, as shown by widespread decreases in cytokine production by G-MDSCs, PMNs, monocytes, and macrophages on day 7 following PJI relative to day 3 post-infection. These findings were corroborated by similar reductions in cytokine, chemokine, and growth factor production at the tissue level. Collectively, this suggests the existence of a critical window during PJI, which may be linked with biofilm formation to elicit changes in leukocyte metabolism and function. Whether this is a host- and/or pathogen-driven phenomenon is unknown and is outside the scope of the current study.
On the other hand, craniotomy infection was characterized by widespread temporal diversity in the mouse model, with each time point and tissue site displaying unique metabolic and functional features. For example, proinflammatory responses in immune cells isolated from the brain parenchyma peaked at day 7 post-infection, typified by a large expansion of activated microglia and increased cytokine production. IL-17 and CXCL10 were also elevated at the tissue level during this interval, which coincided with adaptive immune cell influx into the brain. These changes were associated with significant reductions in bacterial burden in the brain beginning at day 7 and extending to day 14 post-infection. Prior studies have explored the interactions between CD4+ T cells and MHCII+ microglia during CNS viral infection74,75 and microglial responses to planktonic S. aureus76,77; however, less is known about the importance of microglial activation during S. aureus biofilm infection in the CNS. In other neuroinflammation models, microglia are critical for CD4+ T cell recruitment to the brain78, antigen presentation79, and T cell activation80,81. Reciprocally, T cells can potentiate microglial activation via proinflammatory cytokine production82 to enhance phagocytosis and bacterial killing83. Therefore, it is possible that the proinflammatory peak in the brain at day 7 post-infection is influenced by a CD4+ T cell-microglial feedback loop to reduce S. aureus titers in the brain during craniotomy infection. However, this possibility remains speculative.
The main objective of this work was to assess the degree of similarity/divergence in the metabolome as well as granulocyte transcriptomes and function in distinct biofilm niches represented by craniotomy and PJI. From a metabolic perspective, purine and pyrimidine metabolites were differentially detected across time and biofilm models. This finding was supported by IPA, where nucleotide catabolism pathways were biased toward galea and PJI tissues relative to brain, and nucleotide salvage was enriched in PJI vs. galea in extracellular metabolite analysis. Nucleotide demand is heightened during periods of cellular stress and oxidative DNA damage that can occur during inflammation84,85,86, and our RNA-seq analysis identified a transcriptional bias in stress pathways such as eIF2 signaling and the unfolded protein response in granulocytes recovered from the mouse craniotomy infection model compared to PJI. This trend was even more dramatic in patient samples, with several stress-related pathways enriched in craniotomy vs. PJI, including nonsense-mediated decay and translation initiation, elongation, and termination. This finding is significant, as eIF2-activated ER stress is induced by unfolded proteins and amino acid starvation, which broadly represses de novo protein synthesis87 and may impact biofilm formation during craniotomy infection in a mechanism distinct from PJI. In addition to global decreases in protein synthesis, eIF2 signaling also augments the expression of a core set of genes related to amino acid transport, including asparagine synthesis/transport88,89. Our transcriptomic and metabolic analysis support this, where transcriptional pathways related to organic acid transport and asparagine metabolism were enriched during craniotomy infection at days 7 and 14, compared to PJI. Therefore, these results identify a unique transcriptional signature, namely transcriptional stress via eIF2, which may influence metabolic and inflammatory differences across models with a bias toward craniotomy infection.
Analysis of extracellular tissue metabolites revealed key shifts in other organic acid species with known immunomodulatory properties. For example, IPA identified glutamate/glutamine pathways enriched at later time points in craniotomy vs. PJI. Glutamine has been shown to promote proinflammatory properties such as phagocytosis in macrophages57,90 and reactive oxygen/nitrogen species production in granulocytes91,92. Additionally, glutamine and glutamate can be rapidly interconverted and serve as important precursors for nucleotide production, in agreement with pathway flux for nucleic acid synthesis pathways at the same time points. Intracellular metabolomic data also identified a bias toward fatty acid metabolism in granulocytes recovered from craniotomy infection, a trend that was confirmed by increased expression of fatty acid transcriptional pathways by RNA-seq. Conversely, elevations in branched-chain amino acids such as valine, as well as the TCA cycle metabolite aconitic acid, were increased over time during PJI. Interestingly, aconitic acid is converted to itaconate, a known immunomodulatory metabolite associated with S. aureus biofilm formation93,94 and immunosuppressive activity95, potentially facilitating an anti-inflammatory bias in the PJI tissue niche.
Differences in granulocyte inflammatory activity were further apparent in functional assays. In terms of G-MDSCs, IL-10 expression progressively increased in the brain and galea over the course of craniotomy infection, whereas IL-10 production by G-MDSCs remained constant during PJI, with proinflammatory cytokines waning at later intervals. However, at the tissue level, IL-10 was reduced in both the infected galea and PJI homogenates over time. These differences between intracellular vs. extracellular cytokine levels may be explained by additional cell types producing a given mediator that is secreted into infected tissues. Cytokine production by PMNs also differed between infection models, with progressive increases in IL-1β expression during craniotomy infection, whereas PMNs infiltrating PJI displayed a continued reduction in IL-6, TNF, and IL-1β. These divergent granulocyte cytokine signatures coincided with transcriptional differences, where granulocytes infiltrating PJI were enriched for PPAR and PD-1/PD-L1 signaling pathways, both of which are linked to anti-inflammatory activity65,66,96,97 and, importantly, were also upregulated in PMNs from human PJI as well as T cells and monocytes, supporting the translational relevance of these findings and converging trends across immune cell lineages. Granulocyte transcriptional profiles in the mouse PJI model were more G-MDSC-like compared to craniotomy granulocytes, which were PMN-like. This is further supported by the finding that the IL-12 signaling and production pathway was significantly increased in PJI granulocytes and our previous work has shown that IL-12 is critical for G-MDSC abundance and bacterial persistence during PJI24. Therefore, differential IL-12 production between PJI and craniotomy infection may promote the G-MDSC bias in the former, which is corroborated here by elevated IL-12 levels in PJI tissue relative to galea. Collectively, these findings support our prior work where granulocyte depletion with anti-Ly6G reduced S. aureus burden during PJI but increased bacterial abundance in craniotomy infection9,26, further underscoring a difference in inflammatory bias. Although G-MDSCs are the main infiltrate during both S. aureus PJI and craniotomy infection in the galea and bone flap, the more proinflammatory nature of granulocytes in the craniotomy tissue microenvironment presumably allows for a greater role in bacterial clearance. Although PMNs are important for preventing bacterial outgrowth during craniotomy infection, a detrimental role for G-MDSCs is still evident by their ability to inhibit PMN antibacterial activity13,26, reflecting a check-and-balance relationship between these granulocyte subsets. The top transcriptional pathway upregulated in craniotomy vs. PJI granulocytes was macrophage alternative activation signaling, suggesting that granulocytes in the galea may reprogram macrophages to inhibit their proinflammatory activity and promote bacterial persistence.
Finally, bacterial burden was shown to decrease over time in all tissue compartments in PJI, but only substantially in the brain during craniotomy infection. Reductions in bacterial abundance may affect the strength of inflammatory signals sensed by leukocytes and, by extension, immune polarization; however, since bacterial burden in the main tissue niches compared head-to-head in this study (galea and PJI tissue) were comparable across all time points (~106–107 CFU) this possibility appears less likely. At large, the findings of altered immune programming in distinct tissue niches reported here may also explain some of the difficulty in generating a S. aureus vaccine36,39,98. Namely, the local tissue milieu can elicit different immune profiles, increasing the complexity of successfully eliciting protective antibacterial responses across the myriad of tissues that S. aureus can cause invasive disease. This has been demonstrated in recent studies where unique immune responses have been observed when S. aureus invades the epidermis vs. dermis in mouse models of cutaneous infection99,100,101,102,103,104.
This study has several limitations. Regarding our in vivo infection models, detailed transcriptional and metabolomic comparisons were only performed with granulocytes recovered from the galea (craniotomy) and PJI tissue since other leukocyte populations were of lower abundance. Therefore, it is likely that additional tissue niche-specific changes occur in other leukocyte subsets that were not captured here. Second, although G-MDSCs and PMNs exhibit a minor degree of overlap based on surface marker expression, our laboratory and others have validated the gating strategy used here to accurately separate these cell types as indicated by enhanced T cell suppression by G-MDSCs compared to PMNs9,26. Furthermore, prior work has compared surface marker expression on peripheral blood PMNs vs. granulocytes infiltrating biofilm infection, which also delineated G-MDSCs from PMNs105. Nevertheless, it remains possible that some minor overlap between these populations may still occur. Since bulk RNA-seq was performed on total granulocytes, this reduced the ability to resolve G-MDSC- or PMN-specific differences between tissue sites. The paucity of immune infiltrates and limited tissue expansion following sham surgery precluded our ability to assess how responses may be influenced by surgery vs. infection. In addition, differences in parenchymal cell composition in each tissue compartment could influence the extracellular metabolome and immune responses to biofilm infection in each niche. While our mouse infection models utilized the same S. aureus strain, some patient samples analyzed in this report were caused by other bacterial species with different virulence attributes that may influence responses. Clinical microbiology results revealed that no patient included in this study had a detectable polymicrobial infection; however, we cannot definitively rule out the presence of other less abundant microbes; therefore, our ability to comment specifically on S. aureus infection in the clinical population was limited. The distinct immune/transcriptomic/metabolomic profiles observed among the tissue niches could be partially influenced by differences in microbial metabolites. It is difficult to accurately capture the S. aureus intracellular metabolome during in vivo growth due to the highly labile nature of S. aureus metabolism106,107,108, where rapid changes would be expected during the time required to recover bacteria ex vivo. However, future studies can explore S. aureus niche-dependent transcriptional profiles in different tissue microenvironments using a bacterial scRNA-seq platform recently developed by our laboratory109 where predictions of metabolic status can be made. Another point relates to the different substrates for biofilm formation between the models, namely a titanium implant vs. native bone in PJI and craniotomy infection, respectively. However, both models were established using the same low inoculum (i.e., 103 CFU) and involve the release of danger-associated molecular patterns that we posit are an important factor in conditioning the local tissue microenvironment to be permissive for biofilm formation. In addition, removal of the bone flap from the cranium, albeit for a short period, can lead to devascularization from disruption of vascular connections, transforming the bone into a pseudo implant. Nevertheless, the differences in biofilm nucleating surfaces could influence some of the differences between the two models observed in this study. Finally, LC–HRMS was used to profile an extensive metabolomic footprint. Individual metabolites of interest can be selected for analysis in future studies using a sensitive and robust targeted multiple reaction monitoring approach with genuine standards.
This work establishes an important tenet regarding S. aureus biofilm infections, that is, no two tissue niches are identical. Despite utilizing biofilm models that were initiated with the same pathogen and infectious inoculum, profound metabolic, transcriptomic, and functional differences were observed that were temporally and spatially heterogeneous. This work also identifies specific targets for further investigation in these models, such as eIF2 activation and nucleotide, amino acid, and lipid flux. As future immunomodulatory therapies are developed to treat infection in the face of growing antimicrobial resistance, considerations related to the nature of the tissue niche and how this impacts leukocyte programming will need to be considered. A one-size-fits-all approach to immune modulation will not likely be effective as no microenvironment, and thus, no two biofilm infections are exactly equivalent.
Methods
Ethics
Animal studies were conducted according to the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health and comply with the Animal Research: Reporting of In Vivo Experiments guidelines. Animal use protocols for mouse craniotomy (#16-123-10) and PJI (#18-013-03) studies were approved by the University of Nebraska Medical Center Institutional Animal Care and Use Committee.
Single-cell RNA-seq analysis was conducted using a portion of two human datasets previously generated by our laboratory and deposited in the GEO database (GSE249319, human craniotomy infection; GSE241739, human PJI). Samples were intraoperatively collected from patients with craniotomy or PJI following informed consent as permitted by the UNMC IRB [IRB #0241-18-EP (Craniotomy) and IRB #0657-13-EP (PJI)]. Subjects were not compensated for their participation. Participant demographics are provided in Table 1, where sex determination was based on self-reporting. Both male and female mice and human subjects were examined in this study, and similar findings are reported for both sexes.
Mouse biofilm infection models
All mice were group-housed at 21–23 °C (22 °C average) and 30–70% humidity (55% average) under 12 h light/dark cycle with free access to food (2019S Teklad Global 19% Protein Extruded Rodent Diet; Inotiv, West Lafayette, IN) and water. S. aureus craniotomy infection was established in male and female 8–10-week-old C57BL/6J mice (RRID:IMSR_JAX:000664)10,12,15. Briefly, ketamine and xylazine were administered to achieve a surgical plane of anesthesia before skin disinfection with betadine. A midline incision of the scalp was made, whereupon a bone flap was created using a high-speed pneumatic drill (Stryker Corporation, Kalamazoo, MI). The bone flap was incubated with 0.5 mL of S. aureus USA300 LAC13C110 diluted to 106/mL in brain-heart infusion broth at 37 °C for 5 min and subsequently rinsed in PBS, blotted dry on a sterile field, and reimplanted. This procedure reliably produces an infectious inoculum of 103 CFU per bone flap10,12,15, which accurately models SSI that progresses to biofilm formation111. The scalp incision was closed using 6-0 nylon suture.
S. aureus PJI was established in male and female 8–10-week-old C57BL/6J mice9,17,24. Mice were anesthetized with ketamine and xylazine prior to skin disinfection with betadine and initial incision of the quadriceps. A secondary incision was made to laterally displace the patellar tendon, and a burr hole was created in the distal end of the femur with a 26-gauge needle. An orthopedic-grade nickel-titanium Kirschner wire (0.6 mm diameter; Custom Wire Technologies, Port Washington, WI) was inserted through the burr hole into the medullary canal, 103 CFU of S. aureus USA300 LAC13C110 was inoculated at the tip of the wire, and the incision was closed with nylon suture. Mice from both models received buprenorphine SR to alleviate any post-surgical pain and were continuously monitored until ambulatory and daily thereafter.
Importantly, these two animal models share identical pathogens, inoculums, approximate surgical duration, and biofilm characteristics8,9,12,105, and mice were obtained from the same colony to minimize microbiome influences and genetic drift between animals. Both surgical procedures are well tolerated, with a mortality rate of <1%, which is mainly attributed to anesthesia complications. Because of limitations with procuring sufficient tissue (for metabolic assays) or granulocytes from animals with sham craniotomy (Supplementary Fig. 1) or arthroplasty24, time course studies were expressed relative to the day 3 post-infection time point.
Tissue collection, processing, and analysis
Mice were euthanized by isoflurane overdose at the indicated intervals post-infection, whereupon tissue samples were extracted9,15,24. Briefly, single-cell suspensions were prepared from the bone flap, subcutaneous inflammatory tissue above the bone flap (galea), and infected brain hemispheres of mice subjected to craniotomy infection, with aliquots taken for bacterial enumeration by serial dilution and tissue supernatants saved for inflammatory mediator analysis. Samples isolated from animals with PJI included the soft tissue surrounding the infected knee joint (PJI tissue), titanium implant, femur, and knee joint (consisting of the patella with associated ligaments, cartilage, and tendons). These samples were weighed and homogenized24 to obtain single-cell suspensions, samples for bacterial enumeration, and supernatants for analysis of inflammatory mediator expression.
Quantification of immune infiltrates and intracellular cytokine staining were performed on the resulting single-cell suspensions from both biofilm infection models at days 3, 7, and 14 post-infection by flow cytometry. Samples were first incubated with TruStain FcX™ (1:500 dilution; RRID:AB_1574975) to limit nonspecific antibody staining. The following antibody panel was used for all samples: CD45-Brilliant Violet 711™ (RRID:AB_2564383), Ly6G-Spark UV™ (RRID:AB_2924466), Ly6C-FITC (RRID:AB_394628), CD11b-Alexa Fluor® 700 (RRID:AB_394628), F4/80-Brilliant Violet 510™ (RRID:AB_2562622), CX3CR1-Brilliant Violet 785™ (RRID:AB_2565938), MHC-II-Brilliant Violet 605™ (RRID:AB_2565894), γδ TCR-PE (RRID:AB_313832), CD4-Pacific Blue™ (RRID:AB_493374), IL-10-PE/Cyanine7 (RRID:AB_11149682), IL-1β-APC-eFluor™ 780 (RRID:AB_2573996), TNF-PerCP/Cyanine5.5 (RRID:AB_961434), and IL-6-APC (RRID:AB_10694868). All surface marker antibodies were used at a 1:250 dilution, while intracellular cytokine antibodies were used at a 1:100 dilution. Cell viability was assessed using a Zombie UV Fixable viability kit (1:1000 dilution; BioLegend, San Diego, CA; Cat #423108). Intracellular staining was performed using the Cyto-Fast™ Fix/Perm Buffer Set (BioLegend; Cat #426803) following a 4 h incubation of cells with 5 μg/mL brefeldin A. AccuCount beads (Spherotech, Lake Forest, IL; Cat #ACBP-100-10; 8.0–12.9 µm) were added to each sample to enable reporting of absolute cell counts. All acquisition was completed on a BD LSR II-G cytometer controlled by BD FACSDiva (version 8.0.1; RRID:SCR_001456) with subsequent analysis using FlowJo (version 10.8.1; RRID:SCR_008520) and the gating strategies in Supplementary Fig. 6. Importantly, this approach accurately separates G-MDSCs from PMNs as validated by T cell suppression assays during both craniotomy and PJI9,26 as well as delineates differential CD11b expression based on levels compared to peripheral blood PMNs105.
Supernatants collected from the brain and galea of mice with craniotomy infection, as well as the soft tissue surrounding the knee and affected joint of animals with PJI, were analyzed using a MILLIPLEX MAP Mouse Cytokine/Chemokine Magnetic Bead Panel that measures 25 different cytokines, chemokines, and growth factors (Premixed 25-Plex, Cat #HT17MG-14K-PX25, Millipore Sigma, Burlington, MA). Homogenates were centrifuged at 20,000 × g for 10 min at 4 °C to remove residual cellular material and assayed according to the manufacturer’s instructions. A MAGPIX® xMAP instrument (Luminex, Austin, TX) was used for analysis with values corrected for total protein content via BCA assay and results analyzed using Belysa® Analyst software (Millipore Sigma).
RNA-seq
Bulk RNA-seq was performed on mouse granulocytes recovered from the galea (craniotomy infection) and soft tissue surrounding the infected knee joint (PJI) at day 7 post-infection. Single-cell suspensions were prepared as described above and sorted by FACS (FACSAria II, BD Biosciences, Franklin Lakes, NJ) to obtain live CD45+Ly6G+ granulocytes. Nine mice were infected for each biofilm model, with cells from three mice pooled into one sample to obtain adequate RNA for sequencing, resulting in three biological replicates. Total RNA was isolated using a Quick-RNA Microprep Kit (Zymo Research, Irvine, CA; Cat #R1050) and RNA sequencing libraries were prepared using the Universal Plus mRNA-seq kit (Tecan, Männedorf, Switzerland) with 40 ng of input RNA. Libraries were quantified with a Qubit-30 Fluorometer and assessed using a fragment analyzer before sequencing on a NextSeq550 (Illumina, San Diego, CA) with 150 mid-output cycles (75 pair-end reads) at a sequencing depth of ~10 million paired reads per sample. All subsequent data processing and analysis were conducted with Partek Flow Genomics Suite (version 12.1.0; RRID: SCR_011860). Reads were checked for quality and trimmed before alignment to the mouse genome. Additional post-alignment quality control (QC) steps were executed to remove features with low read counts, and data were normalized by counts per million plus 1 × 10−4. DESeq2 was used to determine differential gene expression with control for false discovery rate112. Genes with p < 0.05 were considered differentially expressed. GSEA was performed in Partek Flow to identify differentially regulated pathways and differential expression results were exported and further interrogated using IPA (version 23.0; RRID:SCR_008653). The resulting dataset has been deposited in the GEO database (GSE252481). This experiment was performed in parallel with other samples for an independent project48, where the craniotomy samples were bioinformatically utilized as a control. These files are listed under the same GEO accession number.
Single-cell RNA-seq analysis was conducted using a portion of two human datasets previously generated by our laboratory and deposited in the GEO database (GSE249319, human craniotomy infection; GSE241739, human PJI)60. For this analysis, three subjects with PJI and four with craniotomy infection were analyzed representing 106,392 high-quality transcriptomes. Briefly, samples were intraoperatively collected from patients with craniotomy or PJI following informed consent as permitted by the UNMC IRB [IRB #0241-18-EP (Craniotomy) and IRB #0657-13-EP (PJI)]. Blood, galea (combined from subgalea and epidural samples), intracranial tissue, and bone flap samples were collected for analysis from subjects with craniotomy infection, and blood and peri-prosthetic tissue samples were collected from patients with PJI. Single-cell suspensions were evaluated using a Luna automated fluorescent cell counter (Logos Biosystems, Annandale, VA) to assess cell viability, density, and debris before single-cell capture with a 10X Genomics instrument. Cells were then lysed, and the resulting RNA was reverse-transcribed and barcoded using a Chromium Single Cell 3′ Reagent Kit (v3.1; 10X Genomics, Pleasanton, CA) according to the manufacturer’s instructions. Illumina-compatible cDNA libraries generated by the 10X Chromium platform were quantified with a Qubit-30 Fluorometer and assessed using a fragment analyzer before loading on a Novaseq6000 instrument at a final concentration of 300 pM for generation of 75 bp pair-end reads. Sequencing was performed to an average depth of 50,000–100,000 reads/cell.
Sequencing data were aligned to the human genome using 10X Genomics Cell Ranger before importing into Partek Flow Genomics Suite (version 12.1.0; RRID: SCR_011860) for the remainder of the analysis. A standard QC pipeline was implemented to safeguard against contamination by low-quality cells/reads. Single-cell count matrices were normalized within Partek Flow using counts per million, add 1, and log base 2 transformed. Cells were individually classified into cell types using scRNA-seq (version 2.14.0), Seurat (version 5.0.1; RRID:SCR_007322), Celldex (version 1.10.1), and SingleR69 (version 2.2.0; RRID:SCR_023120) packages with RStudio (version 2024.04.2 build 764; RRID:SCR_000432) and R project for statistical computing (version 4.3.1; RRID:SCR_001905); the Human Primary Cell Atlas68 was used as a reference dataset. These identities were then imported into Partek Flow and used to filter for individual cell types before comparative analysis between cell populations from the galea and PJI tissue. A Hurdle model was used to determine differential gene expression between samples113. Differential expression results were exported and further explored using IPA (version 23.0; RRID:SCR_008653).
Metabolomics
The intracellular metabolome of granulocytes isolated from the galea and PJI tissue of mouse craniotomy and PJI models, respectively, were profiled by LC–HRMS. Fifteen mice were infected for each biofilm model (craniotomy and PJI) with single-cell suspensions prepared by pooling tissue homogenates from three mice into one sample, resulting in five biological replicates. Samples were then enriched for granulocytes using Ly6G magnetic beads (Miltenyi Biotec, Bergishch Gladbach, Germany). Magnetic beads were utilized for purification instead of FACS to limit alterations in cellular metabolism that may occur with extended processing times. Samples were washed twice in 1× PBS, resuspended in 80% MetOH, and frozen at −80 °C for 15 min. Resulting cell lysates were pelleted, supernatant collected and dried by vacuum centrifugation, and stored at −80 °C until submission for LC–HRMS analysis. The resulting pellet was saved for protein quantification and standardization of metabolite peak areas.
Metabolomics was also performed on supernatants prepared from brain, galea, and PJI tissue homogenates at days 3, 7, and 14 post-infection. Similar to granulocyte intracellular metabolite collection, tissue supernatants were centrifuged at high speed to remove residual cellular material, combined with 100% MetOH to yield an 80% MetOH solution, and frozen at −80 °C. A 13C15N-labeled canonical amino acid (13C15N-CAA) mix (Cambridge Isotope Laboratories, Andover, MA) was added to the extraction buffer as an internal standard. Samples were then pelleted, and supernatants were dried by vacuum centrifuge for storage at −80 °C. Cell pellets were stored for protein quantification to normalize metabolite peak areas.
Prior to LC–HRMS, samples were reconstituted in 100 µL of 50% MetOH, pelleted, and the resulting supernatant was submitted for analysis. For QC, 20 µL from each sample was pooled and injected as five technical replicates before and after the sample run. The 13C15N-CAA internal standards in these pooled samples were used to determine instrument stability during the sample run (relative standard deviation; RSD < 15%). The remaining metabolites in the pooled samples were used to filter out metabolites in the individual samples that did not meet the QC threshold (>25% RSD). Untargeted metabolomics was performed using a high-resolution (Tribid) mass spectrometer (Orbitrap viz., Exploris 480; Thermo Fisher Scientific, Waltham, MA) connected with an ultra-high-performance liquid chromatography (UHPLC) system (Thermo Fisher Scientific). Metabolite separation was performed by liquid chromatography using a XBridge Amide analytical column (150 × 2.1 mm ID; 1.7 µm particle size; Waters Corporation, Milford, MA) and a binary solvent system infused at a flow rate of 0.3 ml/min. A guard XBridge Amide column (20 × 2.1 mm ID; 3.5 µm particle size; Waters Corporation) was connected in front of the analytical column. Mobile phase A was composed of ammonium acetate and ammonium hydroxide (10 mM each) containing 5% acetonitrile in LC–MS grade water; mobile phase B was 100% LC–MS grade acetonitrile. The pH of mobile phase A was adjusted to 8.0 using glacial acetic acid. The UHPLC pumps were operated in gradient mode. The amide column was maintained at 40 °C, and the autosampler temperature was held at 5 °C throughout data acquisition. The injection volume for all samples was 5 µl with the 13C15N-CAA mix as the internal standard.
A HRMS Orbitrap (Exploris 480; Thermo Fisher Scientific) was operated in polarity switching mode and was used for untargeted metabolomics in a data-dependent MS/MS acquisition mode (DDA). Electrospray ionization parameters were optimized as follows: electrospray ion voltage of −2700 and 3500 V in negative and positive mode, respectively, ion transfer tube temperature was maintained at 400 °C, and m/z scan range was 70–1050 Da. Orbitrap resolution for precursor ion scans was maintained at 240,000 for intracellular and 120,000 for extracellular samples whereas fragment ion scan resolution was maintained at 120,000 and 60,000 for intracellular and extracellular samples, respectively. Normalized collision energies at 30, 50, and 150% were used for fragmentation and data were acquired in profile mode.
Metabolites were detected within a mass tolerance limit of 5 ppm. Precursor ions generating MS/MS spectra using data-dependent acquisition (DDA) for preferred ions were selected for further analysis. Identification and detection of all metabolites was aided by the Compound Discoverer (CD) software (version 3.3; Thermo Fisher Scientific) using a workflow that included Predicted composition, Metabolomika search, mzCloud, and an internal MassList database containing 4400 metabolites from Thermo Fisher Scientific (Supplementary Data 1). Additionally, the HMDB and KEGG database plug-ins within the CD software were utilized to screen for endogenous metabolites.
The generated data were normalized to the internal standard and protein concentration before analysis by MetaboAnalyst 5.062,114. QEA was also performed using MetaboAnalyst62 to identify biologically meaningful pathways. This technique utilizes relative metabolite abundance data generated from LC–HRMS to identify pathways with overrepresented changes in metabolite concentration across indicated comparisons. Data were further analyzed using IPA (RRID:SCR_008653) and imported into GraphPad Prism (RRID:SCR_002798) for visualization. All raw metabolomic data are deposited in the Metabolomics Workbench Repository (Project ID: PR002139) for use by the community.
Statistics
Significant differences between groups for flow cytometry assays, inflammatory mediator analysis, or metabolomics were determined using an unpaired two-tailed Student t-test, one- or two-way ANOVA with Tukey’s or Šídák multiple comparison test (when required), mixed-effects model with Geisser–Greenhouse correction and Tukey’s multiple comparison test, or Kruskal–Wallis test using GraphPad Prism (RRID:SCR_002798) or MetaboAnalyst 5.062,114. All measurements were taken from distinct samples, and no samples were measured repeatedly. Outliers were only identified for Milliplex assays using the ROUT method (with Q = 1%) in GraphPad Prism115 and removed from analysis. A p value of <0.05 was used to identify statistical significance. For RNA-seq and metabolomic analysis, significant differences were determined using an FDR-adjusted p value of <0.05. Figures were created through Partek Flow, GraphPad Prism, or BioRender.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All scRNA-seq data generated in this study have been deposited in the GEO database under accession codes GSE252481, GSE249319, and GSE241739. All metabolomic data generated in this study have been deposited in the Metabolomics Workbench repository under study IDs ST003482 (intracellular data) and ST003483 (extracellular data), with both studies linked under Project ID PR002139 [https://doi.org/10.21228/M84F91]. The experimental data generated in this study are provided in the Source Data file. Source data are provided with this paper.
References
Mengistu, D. A. et al. Global incidence of surgical site infection among patients: systematic review and meta-analysis. Inquiry 60, 469580231162549 (2023).
Zhang, Z. et al. Epidemiology of patients with central nervous system infections, mainly neurosurgical patients: a retrospective study from 2012 to 2019 in a teaching hospital in China. BMC Infect. Dis. 21, 826 (2021).
Wang, L.-Y. et al. Risk factors for intracranial infection after craniotomy: a case-control study. Brain Behav. 10, e01658 (2020).
Chen, Y. et al. Evaluation of neurosurgical implant infection rates and associated pathogens: evidence from 1118 postoperative infections. Neurosurg. Focus 47, E6 (2019).
Owens, C. D. & Stoessel, K. Surgical site infections: epidemiology, microbiology and prevention. J. Hosp. Infect. 70, 3–10 (2008).
van Belkum, A. et al. Co-evolutionary aspects of human colonisation and infection by Staphylococcus aureus. Infect. Genet. Evol. 9, 32–47 (2009).
Cheung, G. Y. C., Bae, J. S. & Otto, M. Pathogenicity and virulence of Staphylococcus aureus. Virulence 12, 547–569 (2021).
Cheatle, J., Aldrich, A., Thorell, W. E., Boska, M. D. & Kielian, T. Compartmentalization of immune responses during Staphylococcus aureus cranial bone flap infection. Am. J. Pathol. 183, 450–458 (2013).
Heim, C. E. et al. Myeloid-derived suppressor cells contribute to Staphylococcus aureus orthopedic biofilm infection. J. Immunol. 192, 3778–3792 (2014).
Aldrich, A. L. et al. Tlr2 and caspase-1 signaling are critical for bacterial containment but not clearance during craniotomy-associated biofilm infection. J. Neuroinflammation 17, 114 (2020).
de Morais, S. D., Kak, G., Menousek, J. P. & Kielian, T. Immunopathogenesis of craniotomy infection and niche-specific immune responses to biofilm. Front. Immunol. 12, 625467 (2021).
Aldrich, A., Kuss, M. A., Duan, B. & Kielian, T. 3D bioprinted scaffolds containing viable macrophages and antibiotics promote clearance of Staphylococcus aureus craniotomy-associated biofilm infection. ACS Appl. Mater. Interfaces 11, 12298–12307 (2019).
Kak, G. et al. Il-10 production by granulocytes promotes Staphylococcus aureus craniotomy infection. J. Neuroinflammation 20, 114 (2023).
Menousek, J. et al. Transcriptional profiling of phagocytic leukocytes and microglia reveals a critical role for reactive oxygen species in biofilm containment during Staphylococcus aureus craniotomy infection. J. Immunol. 209, 1973–1986 (2022).
Van Roy, Z., Shi, W., Kak, G., Duan, B. & Kielian, T. Epigenetic regulation of leukocyte inflammatory mediator production dictates Staphylococcus aureus craniotomy infection outcome. J. Immunol. https://doi.org/10.4049/jimmunol.2300050 (2023).
Medina, E. & Hartl, D. Myeloid-derived suppressor cells in infection: a general overview. J. Innate Immun. 10, 407–413 (2018).
Heim, C. E. et al. Lactate production by staphylococcus aureus biofilm inhibits hdac11 to reprogramme the host immune response during persistent infection. Nat. Microbiol. 5, 1271–1284 (2020).
Kherabi, Y. et al. Streptococcal and Staphylococcus aureus prosthetic joint infections: Are they really different? BMC Infect. Dis. 22, 555 (2022).
Zimmerli, W., Trampuz, A. & Ochsner, P. E. Prosthetic-joint infections. N. Engl. J. Med. 351, 1645–1654 (2004).
Benito, N. et al. The different microbial etiology of prosthetic joint infections according to route of acquisition and time after prosthesis implantation, including the role of multidrug-resistant organisms. J. Clin. Med. 8 https://doi.org/10.3390/jcm8050673 (2019).
Tornero, E. et al. Prosthetic joint infections due to Staphylococcus aureus and coagulase-negative staphylococci. Int. J. Artif. Organs 35, 884–892 (2012).
Koh, C. K. et al. Periprosthetic joint infection is the main cause of failure for modern knee arthroplasty: an analysis of 11,134 knees. Clin. Orthop. Relat. Res. 475, 2194–2201 (2017).
Heim, C. E. et al. Human prosthetic joint infections are associated with myeloid-derived suppressor cells (mdscs): implications for infection persistence. J. Orthop. Res. 36, 1605–1613 (2018).
Heim, C. E. et al. Il-12 promotes myeloid-derived suppressor cell recruitment and bacterial persistence during Staphylococcus aureus orthopedic implant infection. J. Immunol. 194, 3861–3872 (2015).
Yamada, K. J. et al. Monocyte metabolic reprogramming promotes pro-inflammatory activity and Staphylococcus aureus biofilm clearance. PLoS Pathog. 16, e1008354 (2020).
Aldrich, A. L., Horn, C. M., Heim, C. E., Korshoj, L. E. & Kielian, T. Transcriptional diversity and niche-specific distribution of leukocyte populations during Staphylococcus aureus craniotomy-associated biofilm infection. J. Immunol. 206, 751–765 (2021).
Gold, C., Kournoutas, I., Seaman, S. C. & Greenlee, J. Bone flap management strategies for postcraniotomy surgical site infection. Surg. Neurol. Int. 12, 341 (2021).
Tande, A. J. & Patel, R. Prosthetic joint infection. Clin. Microbiol. Rev. 27, 302–345 (2014).
Ricciardi, B. F. et al. Staphylococcus aureus evasion of host immunity in the setting of prosthetic joint infection: biofilm and beyond. Curr. Rev. Musculoskelet. Med. 11, 389–400 (2018).
Sadhwani, N. et al. Comparison of infection rates following immediate and delayed cranioplasty for postcraniotomy surgical site infections: results of a meta-analysis. World Neurosurg. 173, 167–175.e162 (2023).
Kandel, C. E. et al. Predictors of treatment failure for hip and knee prosthetic joint infections in the setting of 1- and 2-stage exchange arthroplasty: a multicenter retrospective cohort. Open Forum Infect. Dis. 6, https://doi.org/10.1093/ofid/ofz452 (2019).
Fischbacher, A. & Borens, O. Prosthetic-joint infections: mortality over the last 10 years. J. Bone Jt. Infect. 4, 198–202 (2019).
Zhang, J. et al. Sepsis and septic shock after craniotomy: predicting a significant patient safety and quality outcome measure. PLoS ONE 15, e0235273 (2020).
Dashti, S. R. et al. Operative intracranial infection following craniotomy. Neurosurg. Focus 24, E10 (2008).
World Health Organization. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report: 2021 (World Health Organization, 2021).
Tsai, C. M., Caldera, J., Hajam, I. A. & Liu, G. Y. Toward an effective Staphylococcus vaccine: Why have candidates failed and what is the next step? Expert Rev. Vaccines 22, 207–209 (2023).
Redi, D., Raffaelli, C. S., Rossetti, B., De Luca, A. & Montagnani, F. Staphylococcus aureus vaccine preclinical and clinical development: current state of the art. New Microbiol. 41, 208–213 (2018).
Miller, L. S., Fowler, V. G., Shukla, S. K., Rose, W. E. & Proctor, R. A. Development of a vaccine against Staphylococcus aureus invasive infections: evidence based on human immunity, genetics and bacterial evasion mechanisms. FEMS Microbiol. Rev. 44, 123–153 (2020).
Armentrout, E. I., Liu, G. Y. & Martins, G. A. T cell immunity and the quest for protective vaccines against Staphylococcus aureus infection. Microorganisms 8, https://doi.org/10.3390/microorganisms8121936 (2020).
Chen, X. & Alonzo, F. Bacterial lipolysis of immune-activating ligands promotes evasion of innate defenses. Proc. Natl. Acad. Sci. USA 116, 3764–3773 (2019).
Hanzelmann, D. et al. Toll-like receptor 2 activation depends on lipopeptide shedding by bacterial surfactants. Nat. Commun. 7, 12304 (2016).
Hewitt, C. R. et al. Major histocompatibility complex independent clonal t cell anergy by direct interaction of Staphylococcus aureus enterotoxin b with the t cell antigen receptor. J. Exp. Med. 175, 1493–1499 (1992).
Forsgren, A. & Sjöquist, J. “Protein a” from S. aureus: I. Pseudo-immune reaction with human γ-globulin. J. Immunol. 97, 822–827 (1966).
Wilde, A. D. et al. Bacterial hypoxic responses revealed as critical determinants of the host-pathogen outcome by TnSeq analysis of Staphylococcus aureus invasive infection. PLoS Pathog. 11, e1005341 (2015).
Bjarnsholt, T. et al. The importance of understanding the infectious microenvironment. Lancet Infect. Dis. 22, e88–e92 (2022).
Hu, W., Troutman, T. D., Edukulla, R. & Pasare, C. Priming microenvironments dictate cytokine requirements for T helper 17 cell lineage commitment. Immunity 35, 1010–1022 (2011).
Müller, D. N., Wilck, N., Haase, S., Kleinewietfeld, M. & Linker, R. A. Sodium in the microenvironment regulates immune responses and tissue homeostasis. Nat. Rev. Immunol. 19, 243–254 (2019).
Van Roy, Z. & Kielian, T. Tumor necrosis factor regulates leukocyte recruitment but not bacterial persistence during Staphylococcus aureus craniotomy infection. J. Neuroinflammation 21, 179 (2024).
Wu, B. et al. Mitochondrial aspartate regulates tnf biogenesis and autoimmune tissue inflammation. Nat. Immunol. 22, 1551–1562 (2021).
Viola, A., Munari, F., Sanchez-Rodriguez, R., Scolaro, T. & Castegna, A. The metabolic signature of macrophage responses. Front. Immunol. 10, 1462 (2019).
Taylor, C. T. & Scholz, C. C. The effect of hif on metabolism and immunity. Nat. Rev. Nephrol. 18, 573–587 (2022).
Qiu, J. et al. Acetate promotes T cell effector function during glucose restriction. Cell Rep. 27, 2063–2074 e2065 (2019).
Peng, M. et al. Aerobic glycolysis promotes T helper 1 cell differentiation through an epigenetic mechanism. Science 354, 481–484 (2016).
Kelly, B. & O’Neill, L. A. Metabolic reprogramming in macrophages and dendritic cells in innate immunity. Cell Res. 25, 771–784 (2015).
Kaushik, D. K. et al. Enhanced glycolytic metabolism supports transmigration of brain-infiltrating macrophages in multiple sclerosis. J. Clin. Investig. 129, 3277–3292 (2019).
Freemerman, A. J. et al. Metabolic reprogramming of macrophages: glucose transporter 1 (glut1)-mediated glucose metabolism drives a proinflammatory phenotype. J. Biol. Chem. 289, 7884–7896 (2014).
Antunes, D. et al. Glutamine metabolism supports the functional activity of immune cells against Aspergillus fumigatus. Microbiol. Spectr. 11, e0225622 (2023).
Afridi, R., Lee, W. H. & Suk, K. Microglia gone awry: linking immunometabolism to neurodegeneration. Front. Cell. Neurosci. 14, 246 (2020).
Horn, C. M. & Kielian, T. Crosstalk between Staphylococcus aureus and innate immunity: focus on immunometabolism. Front. Immunol. 11, 621750 (2020).
Horn, C. M. et al. Granulocytic myeloid-derived suppressor cell activity during biofilm infection is regulated by a glycolysis/HIF1a axis. J. Clin. Investig. 134, https://doi.org/10.1172/JCI174051 (2024)
O’Neill, L. A. A broken krebs cycle in macrophages. Immunity 42, 393–394 (2015).
Pang, Z. et al. Using MetaboAnalyst 5.0 for LC–HRMS spectra processing, multi-omics integration and covariate adjustment of global metabolomics data. Nat. Protoc. 17, 1735–1761 (2022).
Wishart, D. S. et al. HMDB 5.0: the human metabolome database for 2022. Nucleic Acids Res. 50, D622–D631 (2021).
Kanehisa, M., Furumichi, M., Tanabe, M., Sato, Y. & Morishima, K. Kegg: new perspectives on genomes, pathways, diseases and drugs. Nucleic Acids Res. 45, D353–d361 (2017).
Wang, J.-C. et al. Elevated levels of PD-L1 on mdscs in patients with Ph (−) myeloproliferative neoplasm. Blood 138, 4591 (2021).
Cheuk, Y. C. et al. Integration of transcriptomics and metabolomics reveals pathways involved in mdsc supernatant attenuation of TGF-β1-induced myofibroblastic differentiation of mesenchymal stem cells. Cell Tissue Res. 390, 465–489 (2022).
Alshetaiwi, H. et al. Defining the emergence of myeloid-derived suppressor cells in breast cancer using single-cell transcriptomics. Sci. Immunol. 5, https://doi.org/10.1126/sciimmunol.aay6017 (2020).
Schmiedel, B. J. et al. Impact of genetic polymorphisms on human immune cell gene expression. Cell 175, 1701–1715.e1716 (2018).
Aran, D. et al. Reference-based analysis of lung single-cell sequencing reveals a transitional profibrotic macrophage. Nat. Immunol. 20, 163–172 (2019).
Smith, H. What happens to bacterial pathogens in vivo? Trends Microbiol. 6, 239–243 (1998).
Brown, S. A., Palmer, K. L. & Whiteley, M. Revisiting the host as a growth medium. Nat. Rev. Microbiol. 6, 657–666 (2008).
DePas, W. H. et al. Exposing the three-dimensional biogeography and metabolic states of pathogens in cystic fibrosis sputum via hydrogel embedding, clearing, and rRNA labeling. mBio 7, https://doi.org/10.1128/mBio.00796-16 (2016).
Xu, Y. et al. In vivo gene expression in a Staphylococcus aureus prosthetic joint infection characterized by rna sequencing and metabolomics: a pilot study. BMC Microbiol. 16, 80 (2016).
Lane, T. E. et al. A central role for CD4+ T cells and rantes in virus-induced central nervous system inflammation and demyelination. J. Virol. 74, 1415–1424 (2000).
Olson, J. K. & Miller, S. D. Microglia initiate central nervous system innate and adaptive immune responses through multiple TLRs1. J. Immunol. 173, 3916–3924 (2004).
Kielian, T., Esen, N. & Bearden, E. D. Toll-like receptor 2 (TLR2) is pivotal for recognition of S. aureus peptidoglycan but not intact bacteria by microglia. Glia 49, 567–576 (2005).
Esen, N. & Kielian, T. Central role for MyD88 in the responses of microglia to pathogen-associated molecular patterns. J. Immunol. 176, 6802–6811 (2006).
Zhang, X. et al. Aged microglia promote peripheral T cell infiltration by reprogramming the microenvironment of neurogenic niches. Immun. Ageing 19, 34 (2022).
Funk, K. E. & Klein, R. S. CSF1R antagonism limits local restimulation of antiviral CD8(+) T cells during viral encephalitis. J. Neuroinflammation 16, 22 (2019).
Wheeler, D. L., Sariol, A., Meyerholz, D. K. & Perlman, S. Microglia are required for protection against lethal coronavirus encephalitis in mice. J. Clin. Investig. 128, 931–943 (2018).
Chhatbar, C. & Prinz, M. The roles of microglia in viral encephalitis: from sensome to therapeutic targeting. Cell. Mol. Immunol. 18, 250–258 (2021).
Rock, R. B. et al. Role of microglia in central nervous system infections. Clin. Microbiol. Rev. 17, 942–964 (2004).
Mariani, M. M. & Kielian, T. Microglia in infectious diseases of the central nervous system. J. Neuroimmune Pharmacol. 4, 448–461 (2009).
Tong, J. et al. When DNA-damage responses meet innate and adaptive immunity. Cell. Mol. Life Sci. 81, 185 (2024).
Tran, D. H. et al. De novo and salvage purine synthesis pathways across tissues and tumors. Cell https://doi.org/10.1016/j.cell.2024.05.011 (2024).
Sahan, A. Z., Hazra, T. K. & Das, S. The pivotal role of DNA repair in infection mediated-inflammation and cancer. Front. Microbiol. 9, https://doi.org/10.3389/fmicb.2018.00663 (2018).
Donnelly, N., Gorman, A. M., Gupta, S. & Samali, A. The eIF2α kinases: their structures and functions. Cell. Mol. Life Sci. 70, 3493–3511 (2013).
Harding, H. P. et al. An integrated stress response regulates amino acid metabolism and resistance to oxidative stress. Mol. Cell 11, 619–633 (2003).
Ameri, K. & Harris, A. L. Activating transcription factor 4. Int. J. Biochem. Cell Biol. 40, 14–21 (2008).
Spittler, A. et al. Influence of glutamine on the phenotype and function of human monocytes. Blood 86, 1564–1569 (1995).
Pithon-Curi, T. C., Levada, A. C., Lopes, L. R., Doi, S. Q. & Curi, R. Glutamine plays a role in superoxide production and the expression of p47phox, p22phox and gp91phox in rat neutrophils. Clin. Sci. 103, 403–408 (2002).
Frauwirth, K. in Glutamine in Clinical Nutrition (eds Rajendram, R. et al.) 55–66 (Springer, New York, 2015).
Tomlinson, K. L. et al. Staphylococcus aureus stimulates neutrophil itaconate production that suppresses the oxidative burst. Cell Rep. 42, 112064 (2023).
Tomlinson, K. L. et al. Staphylococcus aureus induces an itaconate-dominated immunometabolic response that drives biofilm formation. Nat. Commun. 12, 1399 (2021).
Li, R., Zhang, P., Wang, Y. & Tao, K. Itaconate: a metabolite regulates inflammation response and oxidative stress. Oxid. Med. Cell. Longev. 2020, 5404780 (2020).
Decara, J. et al. Peroxisome proliferator-activated receptors: experimental targeting for the treatment of inflammatory bowel diseases. Front. Pharmacol. 11, https://doi.org/10.3389/fphar.2020.00730 (2020).
Jun, H. S., Weinstein, D. A., Lee, Y. M., Mansfield, B. C. & Chou, J. Y. Molecular mechanisms of neutrophil dysfunction in glycogen storage disease type Ib. Blood 123, 2843–2853 (2014).
Goldmann, O. & Medina, E. Staphylococcus aureus strategies to evade the host acquired immune response. Int. J. Med. Microbiol. 308, 625–630 (2018).
Cho, J. S. et al. Neutrophil-derived IL-1β is sufficient for abscess formation in immunity against Staphylococcus aureus in mice. PLoS Pathog. 8, e1003047 (2012).
Matsumoto, M. et al. Interaction between Staphylococcus Agr virulence and neutrophils regulates pathogen expansion in the skin. Cell Host Microbe 29, 930–940.e934 (2021).
Liu, H. et al. Staphylococcus aureus epicutaneous exposure drives skin inflammation via IL-36-mediated T cell responses. Cell Host Microbe 22, 653–666.e655 (2017).
Beesetty, P. et al. Tissue specificity drives protective immunity against staphylococcus aureus infection. Front. Immunol. 13, https://doi.org/10.3389/fimmu.2022.795792 (2022).
Lee, B., Olaniyi, R., Kwiecinski, J. M. & Wardenburg, J. B. Staphylococcus aureus toxin suppresses antigen-specific T cell responses. J. Clin. Investig. 130, 1122–1127 (2020).
Si, Y. et al. Inhibition of protective immunity against Staphylococcus aureus infection by MHC-restricted immunodominance is overcome by vaccination. Sci. Adv. 6, eaaw7713 (2020).
Heim, C. E., West, S. C., Ali, H. & Kielian, T. Heterogeneity of Ly6G+ Ly6C+ myeloid-derived suppressor cell infiltrates during Staphylococcus aureus biofilm infection. Infect. Immun. 86, e00684–00618 (2018).
Onyango, L. A. & Alreshidi, M. M. Adaptive metabolism in Staphylococci: survival and persistence in environmental and clinical settings. J. Pathog. 2018, 1092632 (2018).
Liebeke, M. & Lalk, M. Staphylococcus aureus metabolic response to changing environmental conditions—a metabolomics perspective. Int. J. Med. Microbiol. 304, 222–229 (2014).
Clements, M. O. & Foster, S. J. Stress resistance in Staphylococcus aureus. Trends Microbiol. 7, 458–462 (1999).
Korshoj, L. E. & Kielian, T. Bacterial single-cell RNA sequencing captures biofilm transcriptional heterogeneity and differential responses to immune pressure. Preprint at bioRxiv https://doi.org/10.1101/2024.06.28.601229 (2024).
Diep, B. A. et al. Complete genome sequence of USA300, an epidemic clone of community-acquired meticillin-resistant Staphylococcus aureus. Lancet 367, 731–739 (2006).
Sandy-Hodgetts, K. et al. Uncovering the high prevalence of bacterial burden in surgical site wounds with point-of-care fluorescence imaging. Int. Wound J. 19, 1438–1448 (2022).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with deseq2. Genome Biol. 15, 550 (2014).
Finak, G. et al. Mast: a flexible statistical framework for assessing transcriptional changes and characterizing heterogeneity in single-cell RNA sequencing data. Genome Biol. 16, 1–13 (2015).
Pang, Z. et al. MetaboAnalyst 5.0: narrowing the gap between raw spectra and functional insights. Nucleic acids Res. 49, W388–W396 (2021).
Motulsky, H. J. & Brown, R. E. Detecting outliers when fitting data with nonlinear regression—a new method based on robust nonlinear regression and the false discovery rate. BMC Bioinform. 7, 123 (2006).
Goeman, J. J., van de Geer, S. A., de Kort, F. & van Houwelingen, H. C. A global test for groups of genes: testing association with a clinical outcome. Bioinformatics 20, 93–99 (2004).
Acknowledgements
The authors acknowledge Rachel Fallet for managing the mouse colony and the UNMC Flow Cytometry and Genomics Core Facilities for assisting with data acquisition. We would also like to sincerely thank the patients for their participation in this study as well as Drs. William Thorell, Kevin Garvin, and Curtis Hartman for providing surgical specimens from craniotomy and PJI patients. We also thank Drs. Gunjan Kak and Lee Korshoj for critical review of the manuscript and assistance with processing specimens from craniotomy infection patients. This work was supported by the National Institute of Neurological Disorders and Stroke (R01 NS107369) and the National Institute of Allergy and Infectious Diseases (R01 AI169788; P01 AI083211, Project 4) to T.K. Fellowship support was provided by UNMC (Z.V). The UNMC Genomics Core receives partial support from the National Institute for General Medical Science (NIGMS; INBRE—P20GM103427-19 and 1P30GM110768-01). Both the UNMC Genomics and Flow Cytometry Research Cores receive support from The Fred & Pamela Buffett Cancer Center Support Grant (P30CA036727). Figures 1A and 3A were created with BioRender.
Author information
Authors and Affiliations
Contributions
Z.V., P.A., and T.K. designed experiments. Z.V., P.A., and B.P.B. conducted experiments. D.S. and V.C.T. performed metabolomic analysis. Z.V. wrote the manuscript. All authors edited and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Van Roy, Z., Arumugam, P., Bertrand, B.P. et al. Tissue niche influences immune and metabolic profiles to Staphylococcus aureus biofilm infection. Nat Commun 15, 8965 (2024). https://doi.org/10.1038/s41467-024-53353-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-53353-8
This article is cited by
-
Interferon-gamma receptor signaling regulates innate immunity during Staphylococcus aureus craniotomy infection
Journal of Neuroinflammation (2025)
-
The role of bacterial metabolism in antimicrobial resistance
Nature Reviews Microbiology (2025)
-
Bacterial single-cell RNA sequencing captures biofilm transcriptional heterogeneity and differential responses to immune pressure
Nature Communications (2024)