Abstract
Dose-limiting toxicity poses a major limitation to the clinical utility of targeted cancer therapies, often arising from target engagement in nonmalignant tissues. This obstacle can be minimized by targeting cancer dependencies driven by proteins with tissue-restricted and/or tumor-restricted expression. In line with another recent report, we show here that, in acute myeloid leukemia (AML), suppression of the myeloid-restricted PIK3CG/p110γ–PIK3R5/p101 axis inhibits protein kinase B/Akt signaling and compromises AML cell fitness. Furthermore, silencing the genes encoding PIK3CG/p110γ or PIK3R5/p101 sensitizes AML cells to established AML therapies. Importantly, we find that existing small-molecule inhibitors against PIK3CG are insufficient to achieve a sustained long-term antileukemic effect. To address this concern, we developed a proteolysis-targeting chimera (PROTAC) heterobifunctional molecule that specifically degrades PIK3CG and potently suppresses AML progression alone and in combination with venetoclax in human AML cell lines, primary samples from patients with AML and syngeneic mouse models.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
Gene expression data for normal and malignant tissues were obtained from the GTEx gene expression dataset and accessed through the Gepia portal. Gene dependency data were obtained from the DepMap dependency dataset. Data analyses were performed using R or GraphPad Prism 8. Genetic and clinical features were explored using star counts and clinical annotation from the Beat AML 1.0 cohort. The Beat AML 1.0 cohort was used also to assess the gene expression of patients with AML with available transcriptomic profiling. Raw counts from the Beat AML 1.0 cohort were available from the NIH GDC portal and genetic and clinical annotations were available from the supplementary information provided in the original article reporting this cohort26. TCGA data were available from the NIH GDC portal. The RNA-seq-based profiling of the AML cell lines treated with ARM165 is available from GSE260759. Queried gene sets were from the MSigDB Hallmark and C2 geneset libraries. The H3K SRA database was accessible under accession number SRP103200. All other data supporting the findings of this study are available from the corresponding author on reasonable request. No custom code was generated in the course of this study. Source data are provided with this paper.
References
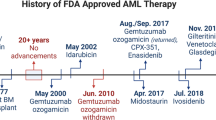
Shimony, S., Stahl, M. & Stone, R. M. Acute myeloid leukemia: 2023 update on diagnosis, risk-stratification, and management. Am. J. Hematol. 98, 502–526 (2023).
Appelbaum, F. R. et al. Age and acute myeloid leukemia. Blood 107, 3481–3485 (2006).
Bhansali, R. S., Pratz, K. W. & Lai, C. Recent advances in targeted therapies in acute myeloid leukemia. J. Hematol. Oncol. 16, 29 (2023).
DiNardo, C. D. et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood 133, 7–17 (2019).
DiNardo, C. D. et al. Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N. Engl. J. Med. 383, 617–629 (2020).
Tsherniak, A. et al. Defining a cancer dependency map. Cell 170, 564–576 (2017).
Burger, J. A. Treatment of chronic lymphocytic leukemia. N. Engl. J. Med. 383, 460–473 (2020).
Jordan, V. C. & O’Malley, B. W. Selective estrogen-receptor modulators and antihormonal resistance in breast cancer. J. Clin. Oncol. 25, 5815–5824 (2007).
Watson, P. A., Arora, V. K. & Sawyers, C. L. Emerging mechanisms of resistance to androgen receptor inhibitors in prostate cancer. Nat. Rev. Cancer 15, 701–711 (2015).
Yu, A. L. et al. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N. Engl. J. Med. 363, 1324–1334 (2010).
Burger, J. A. et al. Long-term efficacy and safety of first-line ibrutinib treatment for patients with CLL/SLL: 5 years of follow-up from the phase 3 RESONATE-2 study. Leukemia 34, 787–798 (2020).
Millis, S. Z., Ikeda, S., Reddy, S., Gatalica, Z. & Kurzrock, R. Landscape of phosphatidylinositol-3-kinase pathway alterations across 19 784 diverse solid tumors. JAMA Oncol. 2, 1565–1573 (2016).
Hirai, H. et al. MK-2206, an allosteric Akt inhibitor, enhances antitumor efficacy by standard chemotherapeutic agents or molecular targeted drugs in vitro and in vivo. Mol. Cancer Ther. 9, 1956–1967 (2010).
Maira, S. M. et al. Identification and characterization of NVP-BKM120, an orally available pan-class I PI3-kinase inhibitor. Mol. Cancer Ther. 11, 317–328 (2012).
Maira, S. M. et al. Identification and characterization of NVP-BEZ235, a new orally available dual phosphatidylinositol 3-kinase/mammalian target of rapamycin inhibitor with potent in vivo antitumor activity. Mol. Cancer Ther. 7, 1851–1863 (2008).
Di Leo, A. et al. Buparlisib plus fulvestrant in postmenopausal women with hormone-receptor-positive, HER2-negative, advanced breast cancer progressing on or after mTOR inhibition (BELLE-3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 19, 87–100 (2018).
Hopkins, B. D. et al. Suppression of insulin feedback enhances the efficacy of PI3K inhibitors. Nature 560, 499–503 (2018).
Krop, I. E. et al. Pictilisib for oestrogen receptor-positive, aromatase inhibitor-resistant, advanced or metastatic breast cancer (FERGI): a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 17, 811–821 (2016).
Furman, R. R. et al. Idelalisib and rituximab in relapsed chronic lymphocytic leukemia. N. Engl. J. Med. 370, 997–1007 (2014).
De Henau, O. et al. Overcoming resistance to checkpoint blockade therapy by targeting PI3Kγ in myeloid cells. Nature 539, 443–447 (2016).
Foubert, P., Kaneda, M. M. & Varner, J. A. PI3Kγ activates integrin α4 and promotes immune suppressive myeloid cell polarization during tumor progression. Cancer Immunol. Res. 5, 957–968 (2017).
Schmid, M. C. et al. Receptor tyrosine kinases and TLR/IL1Rs unexpectedly activate myeloid cell PI3kγ, a single convergent point promoting tumor inflammation and progression. Cancer Cell 19, 715–727 (2011).
Kaneda, M. M. et al. PI3Kγ is a molecular switch that controls immune suppression. Nature 539, 437–442 (2016).
Hong, D. S. et al. Eganelisib, a first-in-class PI3Kγ inhibitor, in patients with advanced solid tumors: results of the phase 1/1b MARIO-1 trial. Clin. Cancer Res. 29, 2210–2219 (2023).
Gu, H. et al. PI3Kγ maintains the self-renewal of acute myeloid leukemia stem cells by regulating the pentose phosphate pathway. Blood 143, 1965–1979 (2024).
Tyner, J. W. et al. Functional genomic landscape of acute myeloid leukaemia. Nature 562, 526–531 (2018).
van Galen, P. et al. Single-cell RNA-seq reveals AML hierarchies relevant to disease progression and immunity. Cell 176, 1265–1281 (2019).
Ng, S. W. et al. A 17-gene stemness score for rapid determination of risk in acute leukaemia. Nature 540, 433–437 (2016).
Cancer Genome Atlas Research, N. et al. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N. Engl. J. Med. 368, 2059–2074, (2013).
Shymanets, A. et al. p87 and p101 subunits are distinct regulators determining class IB phosphoinositide 3-kinase (PI3K) specificity. J. Biol. Chem. 288, 31059–31068 (2013).
Stephens, L. R. et al. The Gβγ sensitivity of a PI3K is dependent upon a tightly associated adaptor, p101. Cell 89, 105–114 (1997).
Horejsi, Z. et al. CK2 phospho-dependent binding of R2TP complex to TEL2 is essential for mTOR and SMG1 stability. Mol. Cell 39, 839–850 (2010).
Sarbassov, D. D., Guertin, D. A., Ali, S. M. & Sabatini, D. M. Phosphorylation and regulation of Akt/PKB by the rictor–mTOR complex. Science 307, 1098–1101 (2005).
Cantley, L. C. The phosphoinositide 3-kinase pathway. Science 296, 1655–1657 (2002).
Pham, L. V. et al. Strategic therapeutic targeting to overcome venetoclax resistance in aggressive B-cell lymphomas. Clin. Cancer Res. 24, 3967–3980 (2018).
Sathe, A. et al. Parallel PI3K, Akt and mTOR inhibition is required to control feedback loops that limit tumor therapy. PLoS ONE 13, e0190854 (2018).
Tavor, S. et al. CXCR4 regulates migration and development of human acute myelogenous leukemia stem cells in transplanted NOD/SCID mice. Cancer Res. 64, 2817–2824 (2004).
Fields, T. A. & Casey, P. J. Signalling functions and biochemical properties of pertussis toxin-resistant G-proteins. Biochem. J. 321, 561–571 (1997).
Houslay, D. M. et al. Coincident signals from GPCRs and receptor tyrosine kinases are uniquely transduced by PI3Kβ in myeloid cells. Sci. Signal. 9, ra82 (2016).
Bondeson, D. P. et al. Lessons in PROTAC design from selective degradation with a promiscuous warhead. Cell Chem. Biol. 25, 78–87 (2018).
Buhimschi, A. D. et al. Targeting the C481S ibrutinib-resistance mutation in Bruton’s tyrosine kinase using PROTAC-mediated degradation. Biochemistry 57, 3564–3575 (2018).
Douglass, E. F. Jr., Miller, C. J., Sparer, G., Shapiro, H. & Spiegel, D. A. A comprehensive mathematical model for three-body binding equilibria. J. Am. Chem. Soc. 135, 6092–6099 (2013).
Wurz, R. P. et al. Affinity and cooperativity modulate ternary complex formation to drive targeted protein degradation. Nat. Commun. 14, 4177 (2023).
Lu, J. et al. Hijacking the E3 ubiquitin ligase Cereblon to efficiently target BRD4. Chem. Biol. 22, 755–763 (2015).
Chua, C. C. et al. Chemotherapy and venetoclax in elderly acute myeloid leukemia trial (CAVEAT): a phase Ib dose-escalation study of venetoclax combined with modified intensive chemotherapy. J. Clin. Oncol. 38, 3506–3517 (2020).
Rahmani, M. et al. Cotargeting BCL-2 and PI3K induces BAX-dependent mitochondrial apoptosis in AML cells. Cancer Res. 78, 3075–3086 (2018).
Lin, K. H. et al. Targeting MCL-1/BCL-XL forestalls the acquisition of resistance to ABT-199 in acute myeloid leukemia. Sci. Rep. 6, 27696 (2016).
Evans, C. A. et al. Discovery of a selective phosphoinositide-3-kinase (PI3K)-γ inhibitor (IPI-549) as an immuno-oncology clinical candidate. ACS Med. Chem. Lett. 7, 862–867 (2016).
Gangadhara, G. et al. A class of highly selective inhibitors bind to an active state of PI3Kγ. Nat. Chem. Biol. 15, 348–357 (2019).
Vanhaesebroeck, B., Ali, K., Bilancio, A., Geering, B. & Foukas, L. C. Signalling by PI3K isoforms: insights from gene-targeted mice. Trends Biochem. Sci. 30, 194–204 (2005).
Nürnberg, B. & Beer-Hammer, S.Function, regulation and biological roles of PI3Kγ variants. Biomolecules 9, 427 (2019).
Perino, A., Ghigo, A., Scott, J. D. & Hirsch, E. Anchoring proteins as regulators of signaling pathways. Circ. Res. 111, 482–492 (2012).
Patrucco, E. et al. PI3Kγ modulates the cardiac response to chronic pressure overload by distinct kinase-dependent and -independent effects. Cell 118, 375–387 (2004).
Beretta, M., Bauer, M. & Hirsch, E. PI3K signaling in the pathogenesis of obesity: the cause and the cure. Adv. Biol. Regul. 58, 1–15 (2015).
Damilano, F., Perino, A. & Hirsch, E. PI3K kinase and scaffold functions in heart. Ann. N. Y. Acad. Sci. 1188, 39–45 (2010).
Mohan, M. L. & Naga Prasad, S. V. Scaffolding function of PI3Kγ emerges from enzyme’s shadow. J. Mol. Biol. 429, 763–772 (2017).
Winter, G. E. et al. Phthalimide conjugation as a strategy for in vivo target protein degradation. Science 348, 1376–1381 (2015).
Bai, L. et al. A potent and selective small-molecule degrader of STAT3 achieves complete tumor regression in vivo. Cancer Cell 36, 498–511 (2019).
Kaneshige, A. et al. A selective small-molecule STAT5 PROTAC degrader capable of achieving tumor regression in vivo. Nat. Chem. Biol. 19, 703–711 (2023).
Koide, E. et al. Development and characterization of selective FAK inhibitors and PROTACs with in vivo activity. Chembiochem 24, e202300141 (2023).
Langmead, B., Trapnell, C., Pop, M. & Salzberg, S. L. Ultrafast and memory-efficient alignment of short DNA sequences to the human genome. Genome Biol. 10, R25 (2009).
Ramirez, F. et al. deepTools2: a next generation web server for deep-sequencing data analysis. Nucleic Acids Res. 44, W160–W165 (2016).
Pohl, A. & Beato, M. bwtool: a tool for bigWig files. Bioinformatics 30, 1618–1619 (2014).
Martz, C. A. et al. Systematic identification of signaling pathways with potential to confer anticancer drug resistance. Sci. Signal. 7, ra121 (2014).
Su, A. et al. The folate cycle enzyme MTHFR is a critical regulator of cell response to MYC-targeting therapies. Cancer Discov. 10, 1894–1911 (2020).
Lin, K. H. et al. P2RY2–Akt activation is a therapeutically actionable consequence of XPO1 inhibition in acute myeloid leukemia. Nat. Cancer 3, 837–851 (2022).
Brinkman, E. K., Chen, T., Amendola, M. & van Steensel, B. Easy quantitative assessment of genome editing by sequence trace decomposition. Nucleic Acids Res. 42, e168 (2014).
Kuo, Y. H. et al. Cbfβ-SMMHC induces distinct abnormal myeloid progenitors able to develop acute myeloid leukemia. Cancer Cell 9, 57–68 (2006).
Pimentel, H., Bray, N. L., Puente, S., Melsted, P. & Pachter, L. Differential analysis of RNA-seq incorporating quantification uncertainty. Nat. Methods 14, 687–690 (2017).
Hanzelmann, S., Castelo, R. & Guinney, J. GSVA: gene set variation analysis for microarray and RNA-seq data. BMC Bioinf. 14, 7 (2013).
Trott, O. & Olson, A. J. AutoDock Vina: improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 31, 455–461 (2010).
Acknowledgements
We thank the members of the A. Puissant, K. C. Wood and A. R. Martin laboratories for their scientific input. We are indebted to V. Montcuquet, N. Setterblad, C. Doliger and C. Maillard from the Saint-Louis Research Institute Core Facility and to CNRS, University Montpellier and the SynBio3 platform supported by IBiSa and the Chimie Balard Cirimat Carnot Institute. We are grateful to L. H. Castilla for providing us with the Cbfb–MYH11 knock-in mouse model and to M. Wymann for providing us with the PIK3CG-directed antibody and for fruitful suggestions on the project. This work was supported by the ERC Starting and Consolidator programs (AltChem 758848 and DynAML 101088563 to A.P.), the Laurette Fugain association (to A.P.), Amgen Innovations (to A.P.), Fondation ARC (to C.Lo.), ATIP-Avenir 2022 Ligue Nationale contre le Cancer (to L. Be.) and the INCA PLBIO program (PLBIO20-246 to A.P. and C.Lo.; PLBIO20-074 to C.Lo.). This work was supported by NIH R01CA266389 (to K.C.W. and A.P.) and NIH U54CA274502 (to A.F., D.L.S. and N.J.K.). M.D. is supported by the Bettencourt Schueller Foundation (CCA-INSERM-Bettencourt). A.P. is an FSER laureate and a recipient of the Brigitte Mérand, Jean Valade and Tourre awards. A.P., R.I., L.Be. and C.L. are supported by the SIRIC InsiTu program (INCa-DGOS-INSERM-ITMO Cancer_18008).
Author information
Authors and Affiliations
Contributions
L.M.K., conceptualization, formal analysis, validation, investigation, visualization, methodology and writing—original draft. J.C.R., conceptualization, formal analysis, validation, investigation, visualization and methodology. K.H.L., conceptualization, formal analysis, validation, investigation, visualization and methodology. F.L., investigation and methodology. M.D., resources and investigation. E.L., investigation and methodology. N.A., investigation and methodology. H.P., resources and methodology. D.H.N., investigation and methodology. J.C., investigation. S.T.K., investigation. H.X.A., investigation. F.N., investigation. C.C., resources. B.L., methodology. D.L., methodology. D.L.S., methodology and resources. N.J.K., resources. L. Brunel, methodology and resources. E.C., methodology and resources. P.V., methodology and resources. M.A., methodology and resources. S.F., resources. T.H., resources. M.S., resources. L.A., resources. E.R., resources. N.F., methodology, resources and support. R.I., conceptualization, methodology and investigation. C.L., conceptualization, formal analysis, visualization and methodology. L. Benajiba, conceptualization, investigation, methodology and resources. A.F., conceptualization, investigation, methodology and visualization. A.R.M., conceptualization, formal analysis, supervision, investigation, visualization, methodology and writing—original draft. K.C.W., conceptualization, supervision, funding acquisition, investigation, visualization, methodology, writing—original draft and project administration. A.P., conceptualization, formal analysis, supervision, funding acquisition, investigation, methodology, writing—original draft and project administration.
Corresponding authors
Ethics declarations
Competing interests
The Krogan Laboratory has received research support from Vir Biotechnology, F. Hoffmann-La Roche and Rezo Therapeutics. N.J.K. has financially compensated consulting agreements with Maze Therapeutics. N.J.K. is the president and on the board of directors of Rezo Therapeutics and a shareholder in Tenaya Therapeutics, Maze Therapeutics, Rezo Therapeutics and Interline Therapeutics. K.C.W. is a cofounder, consultant and equity holder at Tavros Therapeutics and Celldom, is a consultant and equity holder at Simple Therapeutics and Decrypt Biomedicine and has performed consulting work for Guidepoint Global, Bantam Pharmaceuticals and Apple Tree Partners. The other authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks Oliver Hantschel, Ross Levine and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1
a. Comparison of the expression levels of PIK3CG and PIK3R5 across AML and healthy tissues. P-values calculated using one-way ANOVA. Error bars represent mean ± SD. b-d. Expression levels of PIK3CG and PIK3R5 in AML patients from various FAB (b) and genetic (c) subcategories, or at diagnosis versus relapse (d). Median with lower and upper hinges corresponding to the first and third quartiles. The lower and upper whiskers represent the lowest and largest value within 1.5 times the lower and upper interquartile, respectively. The points represent individual values. P-values calculated using two-sided Wilcoxon test and reported on the figure panel. e and f. Spearman correlation between AML cell differentiation state and the expression of PIK3CG and PIK3R5. Correlation between PIK3CG or PIK3R5 expression and ssGSVA score were tested using Spearman’s rank correlation. Two-sided p-values were corrected for multi-testing using the Benjamini & Hochberg method. f. The smooth area corresponds to the 95% confidence interval of the linear regression model. b-f. Data generated using the Beat AML cohort. a-d: n values displayed on the graph.
Extended Data Fig. 2
a. DNA sanger sequencing of the PIK3CG and PIK3R5 genomic regions targeted by the CRISPR-Cas9 PIK3CG- and PIK3R5-directed guides in OCI-AML2 cells. Sequences were aligned using TIDE online tool to determine the relative efficiency of each sgRNA. Repeated twice with similar results. b. Bioluminescence pictures of three representative mice from Fig. 1j injected with OCI-AML2 infected with either a non-targeting control or a PIK3CG-directed sgRNA. Median bioluminescence is depicted in radiance on days 7, 13, 18 and 22.
Extended Data Fig. 3
a and b. Representative growth inhibition curves, and corresponding IC50 and AUC values (n = 4, A, n = 7, B, mean ± SD after three days of seeding) from Fig. 2c of OCI-AML2 cells transduced with either a non-targeting control, two PIK3CG-directed, or two PIK3R5-directed sgRNAs and treated with increasing concentrations of the indicated targeted therapies or chemotherapy drugs (a), FLT3 inhibitors, gilteritinib and sorafenib, or KIT inhibitors, amuvanib and telatinib (b). Av. = Averaged. c. Bioluminescence pictures of three representative mice from Fig. 2i injected with OCI-AML2 cells harboring a non-targeting control or PIK3CG-directed sgRNA. Median bioluminescence is depicted in radiance on days 17, 24, 27 and 31.
Extended Data Fig. 4
a. Volcano plots of the PIK3R5-interacting protein pulled down in OCI-AML2, MV4-11, and NOMO-1 cells compared to control. DIA MS data were processed using Spectronaut with default factory setting providing an unpaired t-test p-value for quantified proteins. b. Ranking of proteins with positive infinite ratios (only identified in PIK3R5 pull down) according to the number of peptides identified. Only proteins with a z-test score > 0.95 were included for further analysis. c. Network corresponding to Fig. 3a depicting, in two colors, the PIK3R5-interacting proteins identified in two cell lines (in yellow) or all three cell lines (in orange).
Extended Data Fig. 5
a. Correlation between gene dependency scores of AKT1 and AKT2 versus PIK3CG in a panel of non-AML cell lines. Data from DepMap CRISPR/Cas9 dependency profiling. Pearson correlation coefficient (ρ) provided to demonstrate no correlation. b. MK-2206 sensitizer and resistor topoisomerase-encoding genes, polymerase-encoding genes, and anti-apoptotic protein-encoding genes identified from a pooled drug-modifier screen conducted in OCI-AML2 cells. Gene-level scores were obtained by averaging sgRNA-level comparisons. Red dot denotes BCL2 identified as a sensitizer gene. All other genes included in the analysis are depicted as blue dots. c. Chemokine/receptor expression heatmap indicating upregulation of both CXCL12/CXCR4 in AML relative to normal tissue. Tumor expression data from TCGA database; normal expression data from GeTex expression database. Data accessed through Gepia gene expression portal.
Extended Data Fig. 6
Synthetic scheme for the synthesis of the PIK3CG degrader, ARM165. Reagents and conditions: i) LiOH monohydrate, MeOH, H2O, 60 °C, 40 h (94%); ii) Boc-AOc-OH, T3P 50% in ethyl acetate, pyridine, N,N-dimethylformamide, 80 °C, 16 h; iii) TFA, CH2Cl2, r.t. 2 h; iv) Glutaric anhydride, N,N-diisopropylethylamine, toluene, N,N-dimethylformamide, 110 °C, 2 h (62% over 3 steps, ii-iv); v) Compound I, HATU, N,N-diisopropylethylamine, N,N-dimethylformamide, r.t. 16 h (55%).
Extended Data Fig. 7
a. Synthetic scheme for the synthesis of non-PIK3CG-targeting control compound for ARM165, ARM204. Reagents and conditions are provided below the synthesis scheme. b. Representative growth inhibition curves with IC50s and AUCs (n = 7, mean ± SD), corresponding to the Fig. 5b for AML and non-AML cells treated with increasing doses of ARM204, AZ2, and ARM165.
Extended Data Fig. 8
a. Representative growth inhibition curves, IC50s, and AUC values n = 7, mean ± SD) corresponding to Fig. 6a of indicated AML cells treated with increasing doses of venetoclax in presence of AZ2 or ARM165 after three days of seeding. b-c. Growth inhibition curves, IC50s, and AUC values (n = 3 biological replicates composed of seven technical replicates, mean ± SD), of OCI-AML2 cells treated with increasing doses of cytarabine, daunorubicin, or venetoclax in combination with 500 nM ARM165. P-values calculated using one-way ANOVA and reported on the figure panel.
Extended Data Fig. 9
a-b. Toxicity profile of ARM165 treatment in naive mice. Mice were treated with IV injection of 0.051 mg/kg ARM165 for seven consecutive days. Individual mouse weight was measured daily (n = 5 mice per group) (a) and the proportion of each indicated hematopoietic cell fraction (b) was established in blood using an MS9 instrument, and in bone marrow (BM) and spleen (SP) by flow cytometry (n = 10 mice per group). Error bars represent mean ± SD. P-values calculated using Mann-Whitney and reported on the figure panel.
Supplementary information
Supplementary Information
Flow cytometry gating strategies.
Supplementary Table 1
Supplementary Table 1: Clinical annotations of the nine primary samples of patients with AML used in the study; female = 0, male = 1. Supplementary Table 2: sgRNA sequences. Supplementary Table 3: Antibodies used for western blot. Supplementary Table 4: shRNA sequences. Supplementary Table 5: Antibodies used for flow cytometry analyses.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data
Unprocessed western blots.
Source Data Extended Data Fig. 1 and Table 1
Statistical source data.
Source Data Extended Data Fig. 3 and Table 3
Statistical source data.
Source Data Extended Data Fig. 4 and Table 4
Statistical source data.
Source Data Extended Data Fig. 5 and Table 5
Statistical source data.
Source Data Extended Data Fig. 6 and Table 6
Drug development data.
Source Data Extended Data Fig. 7 and Table 7
Statistical source and drug development data.
Source Data Extended Data Fig. 8 and Table 8
Statistical source data.
Source Data Extended Data Fig. 9 and Table 9
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kelly, L.M., Rutter, J.C., Lin, K.H. et al. Targeting a lineage-specific PI3Kɣ–Akt signaling module in acute myeloid leukemia using a heterobifunctional degrader molecule. Nat Cancer 5, 1082–1101 (2024). https://doi.org/10.1038/s43018-024-00782-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-024-00782-5
This article is cited by
-
Design and in vitro evaluation of novel tetrazole derivatives of dianisidine as anticancer agents targeting Bcl-2 apoptosis regulator
Scientific Reports (2025)
-
Integrating machine learning and multi-omics analysis to unveil key programmed cell death patterns and immunotherapy targets in kidney renal clear cell carcinoma
Scientific Reports (2025)
-
Inhibiting PI3Kγ in acute myeloid leukemia
Nature Cancer (2024)