Abstract
Immune exhaustion corresponds to a loss of effector function of T cells that associates with cancer or chronic infection. Here, our objective was to decipher the mechanisms involved in the immune suppression of myeloid-derived suppressor cells (MDSCs) and to explore the potential to target these cells for immunotherapy to enhance checkpoint blockade efficacy in a chronic parasite infection. We demonstrated that programmed cell-death-1 (PD-1) expression was significantly upregulated and associated with T-cell dysfunction in advanced alveolar echinococcosis (AE) patients and in Echinococcus multilocularis-infected mice. PD-1 blockade ex vivo failed to reverse AE patients’ peripheral blood T-cell dysfunction. PD-1/PD-L1 blockade or PD-1 deficiency had no significant effects on metacestode in mouse model. This was due to the inhibitory capacities of immunosuppressive granulocytic MDSCs (G-MDSCs), especially in the liver surrounding the parasite pseudotumor. MDSCs suppressed T-cell function in vitro in an indoleamine 2, 3 dioxygenase 1 (IDO1)-dependent manner. Although depleting MDSCs alone restored T-cell effector functions and led to some limitation of disease progression in E. multilocularis-infected mice, combination with PD-1 blockade was better to induce antiparasitic efficacy. Our findings provide preclinical evidence in support of targeting MDSC or combining such an approach with checkpoint blockade in patients with advanced AE.
Similar content being viewed by others
Introduction
Immune exhaustion corresponds to a loss of effector function of T cells that is associated with cancer or chronic infection1. Exhausted T cells exhibit high and sustained expression of inhibitory molecules such as cytotoxic T-lymphocyte-associated protein 4 (CTLA4), programmed cell death 1 (PD-1), T-cell immunoreceptor with Ig and ITIM domains (TIGIT) and lymphocyte activation gene-3 (LAG3)2. Interference with checkpoint inhibitors has revolutionised the field of cancer therapy3,4,5. However, resistance to checkpoint blockade may limit the efficacy of these treatments, and the mechanisms involved in this resistance are not fully understood6. Parasite infections may be used as models to further decipher the mechanisms of resistance and thus find complementary treatments that can restore sensitivity to checkpoint blockade. Parasites such as Schistosoma mansoni (S. mansoni), Leishmania infantum, and Taenia crassiceps (T. crassiceps) have been shown to suppress effective immune responses by upregulating PD-1/PD-1 ligands (PD-L1) on host macrophages or myeloid-derived suppressor cells (MDSCs), which, in turn, inhibit activated T cells7. Recent reports have shown that Echinococcus multilocularis (E. multilocularis) infection is associated with the expression of “checkpoint” receptors which limit the activity of parasite-specific lymphocytes8,9,10. Upregulation of PD-1 is associated with immunosuppression in the livers of infected mice, and in vivo PD-1 blockade enhances host immune responses to control E. multilocularis growth at the early and middle stages of infection11,12; however, the efficacy of PD-1 or PDL1 blockade at late stages of infection remains to be demonstrated. Our recent data also showed that TIGIT and LAG3 function as checkpoints to mediate T-cell exhaustion in the process of E. multilocularis immune escape at the late stage of infection9,10. In addition, we found that TIGIT+ T cells exhibited increased PD-1 expression in patients with alveolar echinococcosis (AE)9. AE is a zoonotic parasitic disease caused by the larvae of E. multilocularis that seriously endangers human health13. AE is characterised by a slow but progressive tumour-like growth of metacestodes (larval stage) mainly in the liver14. The role of immunosuppression in the control of E. multilocularis development has been demonstrated in experimental models and in individuals with impaired immunity, such as AIDS patients or patients who underwent transplantation or were treated with immunosuppressive drugs or biological agents14. The variable clinical outcomes of AE patients depend on the immunological status of host cells, and we and others found that the specific immunological profile associated with T-cell functional impairment plays an important role in the established tolerance state in chronic AE8,15,16. Currently, AE treatment relies only on surgery and albendazole antiparasitic treatment. In addition to allowing us to study the mechanisms of checkpoint blockade, using the ‘E. multilocularis model’ may provide a therapeutic paradigm for treating AE patients.
Multiple suppressive mechanisms, including the accumulation of MDSCs, have been implicated in chronic inflammation and also play a major role in the negative regulation of immune responses during infection and cancer6,17. Mounting evidence has shown that MDSCs, which are the major immunosuppressive cells residing within the hepatic immune microenvironment, are characterised by their ability to contribute to T-cell exhaustion through multiple pathways in chronic inflammation, such as the secretion of arginase 1 (Arg-1), nitric oxide synthase 2 (Nos2 or iNOS) and indoleamine 2, 3-dioxygenase (IDO) or the expression of immunoregulatory molecules18,19,20,21,22. An increase in the MDSC count is related to PD-1 or PD-L1 inhibitor resistance during cancer, infection, and autoimmunity23,24,25. Furthermore, MDSCs expand during helminth infection and may contribute to the immunosuppressive and chronic characteristics of infections caused by S. japonicum, T. crassiceps or Heligmosomoides polygyrus bakeri26. Interfering with the function of MDSC alone or in combination with checkpoint blockade may represent a potentially effective therapeutic approach for eliminating adult worms and inducing immunity to reinfection26. Previous studies have indicated that MDSCs play a key role in downregulating the immune response of T cells in a mouse model of Echinococcus granulosus (E. granulosus) infection27,28. However, the involvement of MDSCs in T-cell dysfunction and their role in resistance to checkpoint blockade has never been studied in E. multilocularis infection.
In this study, we analysed the PD-1 expression profile and functional roles of PD-1 in intrahepatic and peripheral T cells in both AE patients and E. multilocularis-infected mice, and then defined the key roles of MDSCs and the resistance mechanisms to PD-1 blockade in anti-echinococcal immunity. We demonstrated that PD-1 blockade failed to reverse the functional exhaustion of T cells in AE patients ex vivo and failed to inhibit liver metacestode growth, due to the compensatory accumulation of immunosuppressive granulocytic MDSCs (G-MDSCs) in the inflamed liver microenvironment in patients with AE and model mice. Depletion of MDSCs alone enhances the T-cell response. In combination with PD-1 blockade, it also significantly reduces metacestode growth. In addition, we found the effects of IDO1 expression in MDSCs on the immunosuppression of T cells in vitro. Our study suggests that such combination therapy or even depleting MDSCs alone represents a promising therapeutic approach for patients with late-stage AE.
Results
High expression of PD-1 and functional exhaustion of T cells in AE patients
We performed a 10 × 5’ single-cell RNA sequencing (scRNA-seq) analysis of CD45+ cells from four donors with AE using paired liver tissues and peripheral blood (blood) from a public database described previously (accession no. HRA000553; https://figshare.com/s/f2a4578be27c2cb767f9). We observed 8 major cell subtypes, namely, CD4+ T cells, CD8+ T cells, B cells, NK cells, NKT cells, monocytes, MDSCs_like and macrophage, each of which were identified by their signature genes (Fig. 1a–d). It was apparent that there were higher proportions of T and NK cells than of other cell subsets in the liver and of monocyte cells in the blood. The results showed that the inhibitory molecule PD-1 was mainly expressed in liver-derived T lymphocytes and exhausted CD8+ T-cell subsets, exhibiting the highest expression in both the liver tissue close to the parasitic lesions (close liver tissue [CLT]) and distant to the lesions (distant liver tissue [DLT]) (Fig. 1e, related statistics). Among the T-cell subclusters, CD4_c12_PDCD1 and CD8_c5_PDCD1, corresponding to exhausted CD4+ T cells and exhausted CD8+ T cells, respectively, were enriched in the CLT and DLT (Fig. 1f–i, related statistics).
a UMAP plot showing the clustering results for 5 major cell types in the high-quality single-cell RNA sequencing data from the PB, DLTs and CLTs of AE patients (n = 4). b Dot plot showing the highly expressed marker genes in each major cell type. The dot size represents the percentage of cells expressing the marker genes in each major cell type, and the dot colour represents the average expression level of the marker genes in each cell type. Blue indicates high expression, while grey indicates low expression. c Stacked histogram showing the percentages of immune cell types among the total immune cells from the PB, DLT and CLT groups. d UMAP plots showing the cellular compositions of PB, DLT and CLT. e Violin plot showing the expression level of PD-1 in the 7 major cell types in the PB, DLT and CLT samples. f UMAP plot showing the distribution of CD4+ T-cell subsets. Each colour represents a CD4+ T-cell subset. The clusters expressing PD-1 are circled. g UMAP plot showing the expression level of PD-1 in 13 subsets of CD4+ T cells. h UMAP plot showing the distribution of CD8+ T-cell subsets. The clusters expressing PD-1 are circled. i UMAP plot showing the expression level of PD-1 in 12 subsets of CD8+ T cells. PB, peripheral blood; DLT, ‘distant’ liver tissue; CLT, ‘close’ liver tissue. Source data are provided as a Source Data file.
We then confirmed the gene expression of PD-1 and its ligands PD-L1 and PD-L2 at the mRNA level by quantitative real-time polymerase chain reaction (qRT-PCR) in liver samples from AE patients. Our results showed that the PD-1, PD-L1 and PD-L2 genes were upregulated in the CLT of AE patients (Supplementary Fig. S1). We also evaluated the expression of PD-1 in T cells through flow cytometry. The percentage, mean fluorescence intensity (MFI) and absolute count of PD-1+CD4+ T cells and PD-1+CD8+ T cells were significantly higher in the CLT than in the DLT according to paired analysis (Fig. 2a, b). PD-1 was colocalized with CD4+ T cells and CD8+ T cells in the CLT, as determined by multiple-colour fluorescence staining of snap-frozen tissue sections (Fig. 2c).
a Representative flow cytometry plots, percentage, MFI (n = 30) and absolute number (n = 16) of liver CD4+ T cells expressing PD-1 in paired CLTs versus DLTs from AE patients. b Representative flow cytometry plots, percentage, MFI (n = 30) and absolute number (n = 15) of liver CD8+ T cells expressing PD-1 in paired CLTs versus DLTs from AE patients. c Representative images from immunofluorescence costaining of DAPI (blue), CD4 or CD8 (green), PD-1 (red), IgG control (green or red) and merged images of liver sections from AE patients (n = 10). Boxed areas show × 200 magnification of histological images. Arrows indicate CD4+PD-1+ T cells or CD8+PD-1+ T cells. The lesion is delimited with a white line. d, e Representative flow cytometry plot and percentage (n = 15) of granzyme B, IFN-γ and TNF-α production by liver CD4+ T cells or CD8+ T cells that do or do not express PD-1 after PMA/ionomycin stimulation in the CLT of AE patients. (a, b, d, e) Data were analysed using a two-tailed paired Student’s t tests. All data are presented as the mean ± SD. n.s., P > 0.05. Source data are provided as a Source Data file.
To understand the influence of PD-1 expression on T-cell functionality, we examined the cytokine profiles of the T cells in the CLTs of AE patients. We observed that liver-infiltrating PD-1+CD4+ T cells and PD-1+CD8+ T cells produced less interferon-gamma (IFN-γ) and tumour necrosis factor-α (TNF-α) than PD-1-CD4+ T cells and PD-1-CD8+ T cells, respectively (Fig. 2d–e). Moreover, we found that peripheral blood CD4+ T cells and CD8+ T cells from AE patients also expressed higher levels of PD-1 than those from healthy donors (HDs) (Fig. 3a, b). In addition, in the blood of AE patients, PD-1+CD4+ T cells and PD-1+CD8+ T cells expressed lower levels of cytokines such as granzyme B, IFN-γ, and TNF-α than PD-1-CD4+ T cells and PD-1-CD8+ T cells respectively (Fig. 3c, d). These results suggested that liver-infiltrating and blood T cells from AE patients expressed higher PD-1 levels, which was associated with functional impairment.
a Representative flow cytometry plots, percentage, MFI or absolute number of CD4+ T cells expressing PD-1 among the PBMCs of HDs (n = 33) and AE patients (n = 33 or n = 25). b Representative flow cytometry plots, percentage, MFI and absolute number of CD8+ T cells expressing PD-1 in PBMCs of HD (n = 34) and AE patients (n = 33 or n = 28). c, d Representative flow cytometry plot and percentage of granzyme B, IFN-γ and TNF-α production in CD4+ T cells or CD8+ T cells that do or do not express PD-1 in the PBMCs of AE patients (n = 25). a, b Data were analysed using a two-tailed unpaired Student’s t tests. c, d Data were analysed using two-tailed paired Student’s t tests. All data are presented as the mean ± SD. n.s., P > 0.05. Source data are provided as a Source Data file.
High PD-1 expression correlates with the functional exhaustion of T cells in murine E. multilocularis infection
In experimental mice, infiltrating lymphocytes surrounding the E. multilocularis inoculum could only be observed at week 2 post-infection, and few protoscoleces (PSCs) from the hepatic portal vein inoculum were still present. At weeks 12 and 24 post-infection, the parasitic pseudotumor mass included many vesicular structures embedded within thick fibrous tissue, and the periphrastic area was composed of inflammatory cells and fibrous tissue (Fig. 4a).
a Histopathological alterations in the livers of mice infected with PSC inocula during the course of infection. H&E staining of liver sections. The original magnification was at 40 ×; the scale bars indicate 500 μm. b Representative flow cytometry plots and percentages of CD4+ T cells expressing PD-1 [phycoerythrin-labelled (PE)] in the livers of uninfected (2 weeks, n = 5; 12 weeks, n = 6; 24 weeks, n = 6) or infected mice (2 weeks, n = 6; 12 weeks, n = 7; 24 weeks, n = 6) during the course of infection (6–7 mice). c Representative flow cytometry plots and percentages of CD8+ T cells expressing PD-1 in the livers of uninfected (2 weeks, n = 5; 12 weeks, n = 6; 24 weeks, n = 6) or infected mice (2 weeks, n = 6; 12 weeks, n = 7; 24 weeks, n = 6) during the course of infection. d MFI of CD4+ T cells or CD8+ T cells expressing PD-1 in the livers of uninfected (n = 6) or infected mice (n = 6) at week 24 post-infection. e, f, g Percentages of CD44+ (n = 4), CD69+ (n = 4) or Ki67+ cells (n = 6) among CD4+ T cells or CD8+ T cells that do or do not express PD-1 (Brilliant Violet 421TM) in the livers of mice at week 24 post-infection. h, i Representative flow cytometry plot and percentage of granzyme B, CD107α, IFN-γ and TNF-α production in CD4+ T cells or CD8+ T cells that do or do not express PD-1 in the livers of mice at week 24 post-infection (n = 6). PSCs: protoscoleces; pv: parasitic vesicle. b–d Data were analysed using two-tailed unpaired Student’s t tests. e–i Data were analysed using a two-tailed paired Student’s t tests. All data are presented as the mean ± SD from each of at least two independent experiments. n.s., P > 0.05. Source data are provided as a Source Data file.
We investigated PD-1 expression on T cells in the livers of infected mice. The percentage of PD-1+CD4+ T cells was significantly increased at weeks 2, 12 and 24, and there was a higher percentage of PD-1+CD4+ T cells after 24 weeks; moreover, PD-1 expression on CD8+ T cells was significantly elevated at 24 weeks (Fig. 4b, c). In addition, the PD-1 MFI of T cells (both CD4+ and CD8+) was higher in infected mice than in uninfected mice at week 24 (Fig. 4d). Furthermore, we analysed the activation and proliferation of CD4+ T cells and CD8+ T cells via the expression of CD44, CD69 and Ki67, and found that PD-1+ T cells (both CD4+ and CD8+) were more activated and proliferative than their PD-1- counterparts after 24 weeks of infection (Fig. 4e–g). We also found that a lower percentage of liver-infiltrating PD-1+ T cells (both CD4+ and CD8+) expressed IFN-γ and TNF-α than PD-1- T cells (Fig. 4h, i).
Consistent with our findings in liver T cells, the percentage of splenic PD-1+ T cells (both CD4+ and CD8+) increased at 24 weeks after E. multilocularis infection (Supplementary Fig. S2a, b). In addition, the PD-1 MFI of CD4+ T cells was higher in infected mice than in control mice at week 24 (Supplementary Fig. S2c). Splenic PD-1+ T cells (both CD4+ and CD8+) were more activated and proliferative than their PD-1- counterparts in mice after 24 weeks of infection (as indicated by the expression of CD69, CD44 and Ki67; Supplementary Fig. S2d–f). Furthermore, splenic PD-1+ T cells (both CD4+ and CD8+) showed significantly impaired cytokine secretion. However, the percentage of splenic PD-1+ T cells (both CD4+ and CD8+) that expressed granzyme B and CD107α was higher than that of PD-1- T cells (Supplementary Fig. S2g, h). Collectively, these results indicated that high PD-1 expression was associated with functional exhaustion of liver and splenic T cells (both CD4+ and CD8+) in late-stage E. multilocularis-infected mice.
PD-1 blockade or deficiency has no direct effect on disease progression or T-cell function in murine E. multilocularis infection
To further evidence the role of PD-1 on T cells (both CD4+ and CD8+) during E. multilocularis infection, we treated E. multilocularis-infected mice with anti-PD-1 mAb or anti-PD-L1 mAb. Anti-PD-1 or anti-PD-L1 blockade alone failed to inhibit the growth of metacestodes (Supplementary Figs. S3a–c, S4a–c), although the percentages of single-positive TNF-α and double-positive TNF-α and IL-2 CD4+ T cells and the percentage of double-positive IFN-γ and TNF-α CD8+ T cells were increased in the livers of anti-PD-1-treated mice (Supplementary Figs. S3d, S5). The percentages of single-positive IL-2 and double-positive TNF-α and IL-2 CD4+ T cells and the percentages of single- or double-positive IFN-γ and IL-2, double-positive IFN-γ and TNF-α CD8+ T cells, and of CD8+ T cells expressing granzyme B, IFN-γ, TNF-α and IL-2, were increased in the spleens of anti-PD-L1-treated mice (Supplementary Fig. S4d). However, the percentages of double-positive TNF-α and IL-2 splenic T cells (both CD4+ and CD8+) and the percentage of single-positive TNF-α splenic CD8+ T cells were significantly lower in anti-PD-1-treated mice than in WT mice (Supplementary Fig. S3e). In addition, PD-1 blockade did not affect the expression of CD69 on T cells or the phenotype of Tem cells (both CD4+ and CD8+) (Supplementary Fig. S3f–i).
Consistent with the results observed in PD-1-blockade mice, we found that PD-1 deficiency did not inhibit liver metacestode growth in infected PD-1-/- mice at 2, 12 and 24 weeks. Whole liver weight and lesion weight were not significantly different between PD-1-/- mice and wild-type (WT) mice (Fig. 5a-c). PD-1-/- mice exhibited a significantly higher percentage of CD69+CD4+ T cells in the liver than WT mice at 24 weeks post-infection. In contrast, PD-1 deficiency did not affect the expression of CD69 on CD8+ T cells or the phenotype of effector memory CD44+CD62L- T cells (Tem, both CD4+ and CD8+) (Fig. 5d, e), which play an essential role in protecting against parasitic infections through its own effector functions such as cytotoxicity and cytokine secretion29,30,31. The percentage of single-positive IFN-γ CD4+ T cells was increased in the livers of PD-1-deficient mice (Fig. 5f). However, the percentages of single- or double-positive TNF-α and IL-2 CD4+ T cells and the percentages of double-positive IFN-γ and IL-2 and triple-positive IFN-γ, TNF-α and IL-2 CD8+ T cells were significantly lower in the livers of PD-1-deficient mice than in those of WT mice (Fig. 5f). Compared with those in WT mice, splenic T cells (both CD4+ and CD8+) in PD-1-/- mice showed no significant activation, effector memory phenotype or degranulation (Supplementary Fig. S6a, b). The percentage of double-positive TNF-α and IL-2 CD4+ T cells was significantly lower in the spleens of PD-1-deficient mice than in those of WT mice (Supplementary Fig. S6c).
a Workflow of the experimental procedure for the PD-1-/- mice and wild type (WT) mice infected with E. multilocularis PSCs. Mice image was drawn by hand with Procreate software. Analysis of liver lesion weight at weeks 2, 12 and 24 post-infection and flow cytometry of T cells in the liver and spleen at week 24 post-infection. b Representative image of metacestode tissue in the livers of wild-type (WT) or PD-1-/- mice at weeks 2, 12, and 24 post-infection. Metacestode tissues are circled in yellow. c Whole liver weight (left) and lesion weight (right) in the livers of WT or PD-1-/- mice at weeks 2 (WT, n = 10; PD-1-/-, n = 12), 12 (WT, n = 10; PD-1-/-, n = 11), and 24 (WT, n = 16; PD-1-/-, n = 10) of persistent infection. d Percentage of CD69+ cells among CD4+ T cells or CD8+ T cells in the livers of WT (n = 5) or PD-1-/- mice (n = 5) at week 24 post-infection. e Percentage of effector memory CD4+ T cells (CD44+CD62L-CD4+ Tem) or CD8+ T cells (CD44+CD62L-CD8+ Tem) in the livers of WT (n = 5) or PD-1-/- mice (n = 5) at week 24 post-infection. f Percentages of CD4+ T cells or CD8+ T cells positively stained for one, two or multiple cytokines (i.e., granzyme B, IFN-γ, TNF-α and IL-2) in the livers of WT (n = 5) or PD-1-/- mice (n = 5) at week 24 post-infection. c–f Data were analysed using two-tailed unpaired Student’s t tests. All data are presented as the mean ± SD from each of at least two independent experiments. n.s., P > 0.05. Source data are provided as a Source Data file.
Importantly, to determine whether in vitro blockade of PD-1 on T cells could reactivate their functional responsiveness, peripheral blood mononuclear cells (PBMCs) were isolated from AE patients and restimulated with anti-CD3e/CD28 in the presence of anti-PD-1 mAb. No significant increase in IFN-γ or TNF-α levels was observed in CD4+ T cells or CD8+ T cells upon the addition of anti-PD-1 mAb, indicating that PD-1 blockade could not restore cytokine secretion by exhausted CD4+ T cells or CD8+ T cells from AE patients ex vivo (Supplementary Fig. S7). Taken together, these data indicated that PD-1 blockade or deficiency could not reverse the exhaustion of T cells in AE patients or mouse models to enhance anti-echinococcal immunity.
MDSCs accumulation and T-cell suppression in AE patients and murine E. multilocularis infection
To determine whether myeloid cell recruitment contributes to immune suppression by inhibiting the T-cell response, we analysed mRNA expression data in paired liver tissue (CLT versus DLT) from 6 AE patients studied in our previous report (accession no. GSE124362). Gene set enrichment analysis (GSEA) revealed a marked upregulation of genes associated with myeloid leukocyte migration in the CLT compared to the DLT (Supplementary Fig. S8a). These upregulated genes were associated with myeloid cell chemotaxis, such as CCL1, CCL2, and CXCR2; myeloid cell activation and expansion, such as VEGFA, S100A8, S100A9, and S100A12; and myeloid leukocyte differentiation, such as CSF3R (Supplementary Fig. S8b). Furthermore, Gene Ontology (GO) analysis revealed that the upregulated genes, including CD33, S100A8, S100A9, IL-10, IDO1, and NOS2 in the CLT from AE patients were enriched in myeloid leukocyte migration, myeloid leukocyte activation, myeloid leukocyte-mediated immunity, which are related to the characteristics, recruitment and immunosuppressive function of MDSCs (Supplementary Fig. S8c–e). Our results also showed that the phenotype and functional markers of G-MDSCs (e.g., CD33, CD11b, CD15, IDO1, S100A8, S110A9, and S100A12) were upregulated at the mRNA level in the whole liver cell mixture from CLTs (Supplementary Fig. S1). Moreover, flow cytometry revealed that the absolute numbers of MDSCs and G-MDSCs were significantly increased in the CLT of AE patients, while the absolute number of monocytic MDSCs (M-MDSCs) was not (Supplementary Fig. 6a–c), in agreement with results from scRNA-seq analysis (Fig. 1a–d).
a Flow cytometric gating strategy used to identify and integrate liver-infiltrating MDSCs, G-MDSCs and M-MDSCs from AE patients. b, c Percentage or absolute number of MDSCs, G-MDSCs and M-MDSCs in paired CLTs versus DLTs from AE patients (n = 11). d Representative flow cytometry plot of MDSCs, G-MDSCs and M-MDSCs in the livers of uninfected, wild-type (WT) or PD-1-/- mice at week 24 post-infection. e, f Percentage or absolute number of MDSCs, G-MDSCs and M-MDSCs in the livers of uninfected, WT or PD-1-/- mice at week 24 post-infection (n = 5). The data represent at least two independent experiments. b, c Data were analysed using two-tailed paired Student’s t tests. e, f Data were analysed using a one-way ANOVA with Tukey’s multiple comparisons test. All data are presented as the mean ± SD. n.s., P > 0.05. Source data are provided as a Source Data file.
We next evaluated the accumulation of local and peripheral MDSCs in WT mice at 24 weeks post-infection. An enrichment of MDSCs (e.g., M-MDSCs) was observed in the liver of WT mice after infection. In addition, splenic MDSCs (both G-MDSCs and M-MDSCs) were more abundant in infected WT mice than in uninfected mice at week 24 (Fig. 6d–f). Importantly, we observed a statistically significant increase in both the percentage and absolute number of MDSCs and G-MDSCs in the liver and spleen of PD-1-/- mice compared to those of WT mice at 24 weeks post-infection. However, there was no significant difference in monocytic MDSCs (M-MDSCs) between PD-1-/- mice and WT mice (Fig. 6d–f and Supplementary Fig. S9a, b). These results suggested that abundant MDSCs, including G-MDSCs, limited the adaptive anti-echinococcal effector function of T cells and that depleting MDSCs alone or in conjunction with anti-PD-1 could be a potential therapeutic strategy to promote PD-1 blockade efficacy while boosting anti-echinococcal immune response.
MDSCs depletion enhances activation and reduces exhaustion of T cell and potentiates the efficacy of PD-1 blockade in murine E. multilocularis infection
We next investigated the role MDSCs and the effect of depleting MDSCs on T cell function and disease progression in chronic E. multilocularis model. The combination of anti-PD-1 and anti-Gr-1 mAb significantly decreased liver metacestode growth, whereas anti-PD-1 monotherapy did not affect growth (Fig. 7a–c). In addition, anti-Gr-1 treatment alone significantly depleted hepatic G-MDSCs, M-MDSCs and splenic G-MDSCs, and partially limited parasite progression in the liver; however, the observed decrease in liver parasite weight was not significant (Supplementary Fig. S10 and Fig. 7a–c). The combined treatment significantly increased the percentages of CD69+CD8+ T cells, liver Tem cells (both CD4+ and CD8+) and splenic CD8+ Tem cells in mice treated with anti-PD-1 or non-related IgG alone. There was also an increase in liver Tem cells (both CD4+ and CD8+), IFN-γ CD4+ T cells and IL-2 CD8+ T cells percentages after anti-Gr-1 treatment alone (Fig. 7d–f and Supplementary Fig. S11a, b). However, significantly greater levels of IFN-γ and IL-2 were produced by liver T cells (both CD4+ and CD8+) following combined treatment than following treatment with anti-PD-1, anti-Gr-1 or non-related IgG alone. In addition, splenic T cells (both CD4+ and CD8+) produced high levels of IFN-γ following the combined treatment (Fig. 7f and Supplementary Fig. S11c). Importantly, anti-Gr-1 treatment elicited a strong synergistic effect with anti-PD-1 to markedly boost the level of IFN-γ in liver T cells (both CD4+ and CD8+) (Fig. 7f). Collectively, these results indicated that depleting MDSCs partially restores effector immunity against E. multilocularis larvae. In addition, it strongly synergises with PD-1 blockade to significantly reverse the exhaustion of T cells, at least partially via the restoration of their IFN-γ and IL-2 production, including locally, in the infected liver.
a Protocol for anti-PD-1 and/or anti-Gr-1 blockade in the late stage of infection. Mice image was drawn by hand with Procreate software. Twelve weeks after E. multilocularis infection, control IgG (2A3), anti-PD-1 mAb (RMP1-14), anti-Gr-1 mAb (RB6-8C5) or a combination of both antibodies were intraperitoneally administered twice a week for an additional 12 weeks. b Representative image of metacestode tissue in the liver of persistently infected mice treated with IgG, anti-PD-1 mAb, anti-Gr-1 mAb or a combination of anti-PD-1 mAb and anti-Gr-1 mAb for 12 weeks starting at week 12 post-infection. Metacestode tissues are circled in yellow. c Whole liver weight and lesion weight in the livers of persistently infected mice treated with non-related IgG (n = 6), anti-PD-1 mAb (n = 5), anti-Gr-1 mAb (n = 5) or a combination of anti-PD-1 mAb and anti-Gr-1 mAb (n = 5) for 12 weeks starting at week 12 post-infection. d Percentage of CD69+ cells among CD4+ T cells or CD8+ T cells in the livers of persistently infected mice treated with non-related IgG (n = 6), anti-PD-1 mAb (n = 5), anti-Gr-1 mAb (n = 5) or a combination of anti-PD-1 mAb and anti-Gr-1 mAb (n = 5). e Percentage of CD4+ Tems or CD8+ Tems in the livers of persistently infected mice treated with non-related IgG (n = 6), anti-PD-1 mAb (n = 5), anti-Gr-1 mAb (n = 5) or a combination of anti-PD-1 mAb and anti-Gr-1 mAb (n = 5). f Percentage of IFN-γ, TNF-α and IL-2 -expressing CD4+ T cells or CD8+ T cells in the livers of persistently infected mice treated with non-related IgG (n = 6), anti-PD-1 mAb (n = 5), anti-Gr-1 mAb (n = 5) or a combination of anti-PD-1 mAb and anti-Gr-1 mAb (n = 5). c–f Data were analysed using a one-way ANOVA with Tukey’s multiple comparisons test. All data are presented as the mean ± SD from each of at least two independent experiments. n.s., P > 0.05. Source data are provided as a Source Data file.
We then targeted MDSCs with anti-Gr-1 mAb starting at 13 weeks in PD-1-/- mice after infection. Whole liver weight and lesion weight were significantly lower in PD-1-/- mice treated with anti-Gr-1 mAb than in PD-1-/- mice (Fig. 8a–c). In addition, the large difference in lesion weight (and total liver weight) within groups is closely related to the growth characteristics of the parasite itself (Fig. 8c). Anti-Gr-1 treatment significantly increased the percentage of liver CD69+CD4+ T cells, splenic CD69+CD8+ T cells and Tem cells (both CD4+ and CD8+) in PD-1-/- mice although the absolute number of liver T cells (both CD4+ and CD8+) showed no increase (Fig. 8d–f and Supplementary Fig. S12a, b). Furthermore, significantly increased percentages of single- or double-positive IFN-γ and IL-2 CD4+ T cells were present among the liver T cells from PD-1-/- mice treated with anti-Gr-1 mAb; significantly increased percentages of double-positive IFN-γ and granzyme B or IL-2, triple-positive IFN-γ, IL-2 and granzyme B or TNF-α CD8+ T cells, and of CD8+ T cells expressing granzyme B, IFN-γ, TNF-α and IL-2, were present in the liver from PD-1-/- mice treated with anti-Gr-1 mAb (Fig. 8g). In addition, high percentages of single-positive IL-2, double-positive IL-2 and IFN-γ or TNF-α, and triple-positive IFN-γ, TNF-α and IL-2 CD4+ T cells were present in the spleen following anti-Gr-1 treatment; high percentages of single- or double-positive IFN-γ and IL-2, double-positive IFN-γ and TNF-α, and triple-positive IFN-γ, IL-2 and granzyme B or TNF-α CD8+ T cells were also present in the spleens of the infected mice following anti-Gr-1 treatment (Supplementary Fig. S12c). These data also showed that abundant MDSCs, including G-MDSCs, limited the adaptive anti-echinococcal effector function of T cells and that depleting MDSCs inhibited metacestode growth in PD-1-deficient mice after infection.
a Protocol for anti-Gr-1 blockade in the late stage of infection. Mice image was drawn by hand with Procreate software. Twelve weeks after E. multilocularis infection of PD-1-/- mice, control IgG (LTF-2) or anti-Gr-1 mAb (RB6-8C5) was intraperitoneally administered two times a week for 12 weeks. b Representative image of metacestode tissue in the liver of persistently infected PD-1-/- mice treated with IgG or anti-Gr-1 mAb for 12 weeks starting at week 12 post-infection. c Whole liver weight (left) and lesion weight (right) in the livers of persistently infected PD-1-/- mice treated with IgG (n = 6) or anti-Gr-1 mAb (n = 6) for 12 weeks starting at week 12 post-infection. d Absolute numbers of CD4+ T cells and CD8+ T cells in the livers of persistently infected PD-1-/- mice treated with IgG (n = 5) or anti-Gr-1 mAb (n = 5). e Percentage of CD69+ cells among CD4+ T cells or CD8+ T cells in the livers of persistently infected PD-1-/- mice treated with IgG (n = 5) or anti-Gr-1 mAb (n = 5). f Percentage of CD4+ Tems or CD8+ Tems in the livers of persistently infected PD-1-/- mice treated with IgG (n = 5) or anti-Gr-1 mAb (n = 5). g Percentage of CD4+ T cells or CD8+ T cells positively stained for one, two or multiple cytokines (i.e., granzyme B, IFN-γ, TNF-α and IL-2) in the livers of persistently infected PD-1-/- mice treated with non-related IgG (n = 5) or anti-Gr-1 mAb (n = 5). c–g Data were analysed using two-tailed unpaired Student’s t tests. All data are presented as the mean ± SD from each of at least two independent experiments. n.s., P > 0.05. Source data are provided as a Source Data file.
G-MDSCs suppress the T-cell response mainly via IDO1 in AE patients and murine E. multilocularis infection
Based on the data presented thus far, we found that the mRNA levels of IDO1 and NOS2 as critical mediators of the suppressive phenomenon, increased in the CLT from AE patients (Supplementary Fig. S8). Immunohistochemistry was subsequently used to determine the protein expression levels of CD33, IDO1 and INOS in liver tissues from AE patients. There were greater numbers of CD33+ cells, IDO1+ cells and INOS+ cells in the inflammatory infiltrate of the periphrastic area in the CLT samples than in the DLT samples (Fig. 9a–d), and the percentages of hepatic CD33+ cells and IDO1+ cells were significantly positively associated with fluorodeoxyglucose (FDG) uptake via positron emission tomography (PET)-CT, a marker of metabolic activity of the lesions in the patient liver; however, the percentage of INOS+ cells was not associated with this marker (Fig. 9e, f). Furthermore, IDO1 was colocalized with CD33+ cells in the CLT (Fig. 9g). We also found that the absolute number of IDO1+ MDSCs was significantly greater in the livers of PD-1-/- mice after 24 weeks of infection (Fig. 9h). These data suggested that MDSCs might impair the function of T cells by producing IDO1.
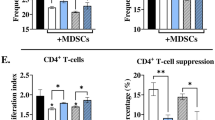
a Representative immunohistochemical staining for CD33, IDO1 or INOS (upper panel 100 ×, lower panel 400×) in liver sections from AE patients (left). Arrowheads indicate CD33+ cells, IDO1+ cells or INOS1+ cells. b, c, d The percentage of positively stained cells was calculated to assess the expression of CD33 (n = 13), IDO1 (n = 15) or INOS (n = 13). e Example of two patients. Patient No.26 with low metabolic activity (PET-CT, SUV = 1.9, left image a) and corresponding staining for CD33 or IDO1 in periphrastic liver tissue (right image, 400 ×). Patient No.63 with high metabolic activity (PET-CT, SUV = 9.4, left image a) and corresponding staining for CD33 or IDO1 in periphrastic liver tissue (right image, 400 ×). Left image (b): Corresponding CT scan; Left Image (c): Corresponding PET/CT fusion image; Left image (d): Corresponding region with radiopharmaceutical distribution in the hepatic lobe, as detected by maximum intensity projection (MIP). Arrows indicate 18F-FDG uptake (hot spots). f Correlations between the percentages of CD33+ cells, IDO1+ cells or INOS+ cells and the FDG-PET uptake value in the perilesional area (n = 14). g Representative images of the immunofluorescence staining for DAPI (blue), CD33 (green), and IDO1 (green) and merged images of liver sections from AE patients (n = 10). Boxed areas show × 200 magnification of histological images. Arrows indicate CD33+ IDO1+ MDSCs. A white line was drawn around the lesion. h Percentage of IDO1+ MDSCs in the livers of wild-type (WT) or PD-1-/- mice at week 24 post-infection (n = 3). i IFN-γ and TNF-α secretion in the supernatant of CD4+ T cells or CD8+ T cells cocultured with G-MDSCs for 48 h in the presence of the control or IDO1 inhibitor (1-MT) was measured by ELISA. The data represent at least two independent experiments. Standard uptake value, SUV. b–d Data were analysed using two-tailed paired Student’s t tests. f Data were analysed using a two-tailed Pearson’s correlation. h Data were analysed using a one-way ANOVA with Tukey’s multiple comparisons test. All data are presented as the mean ± SD. n.s., P > 0.05. Source data are provided as a Source Data file.
To further verify that IDO1 was indeed important for suppression, we measured T-cell function in G-MDSCs obtained from the spleens of E. multilocularis-infected mice in the presence of an IDO1inhibitor in vitro. There was a significant increase in IFN-γ and TNF-α levels after the addition of 1-methyl-Trp (1-MT), confirming that G-MDSCs exert their suppressive effects through the expression of IDO1 (Fig. 9i).
Discussion
The T-cell population is one of the main contributors to resistance against tumours, intracellular viruses and parasitic infection32,33. The functional deficiency of T cells is associated with pathogen progression and contributes to disease pathogenesis9,16,34 In the present study, a late-stage E. multilocularis infection model is used to better understand the mechanisms involved in resistance to checkpoint blockade and how this resistance might be overcome by combined specific biotherapy. The results demonstrated that reversing checkpoint inhibition is not sufficient to restore an efficient immune response by the host and that MDSCs are also key actors, at least partially by an IDO1-dependent mechanism, and should be targeted simultaneously to alleviate the deleterious effect of T-cell exhaustion on the progression of AE lesions. Moreover, targeting MDSCs alone showed a certain level of therapeutic potential. These findings are consistent with those obtained through other models of T-cell exhaustion and checkpoint inhibition, such as malignant tumours or other types of infection20,23,25. In addition, they provide experimental evidence for the ability of MDSCs-based therapy and especially of therapies which combine checkpoint blockadeand MDSC-targeting to treat patients with a life-threatening parasitic disease.
PD-1 is a central regulator of T-cell exhaustion, a state of T-cell dysfunction that may occur during many chronic infections. With regard to echinococcosis, PD-1 was found to be highly expressed in the hepatic T cells of AE patients and mice infected with E. multilocularis9,35. Significantly higher levels of sPD-L1 were observed in patients with cystic echinococcosis (CE) than in healthy controls36, which suggests that sPD-L1 levels can be a predictive biomarker of recurrence after surgery37. In this study, we demonstrated that upregulation of PD-1 expression leads to T-cell exhaustion in the liver, blood and spleen as E. multilocularis infection progresses to the chronic stage. However, our study revealed that PD-1-deficient mice or anti-PD-1/anti-PD-L1 treatment failed to control established metacestode at such later stages (12–24 weeks). In addition, PD-1 blockade did not restore cytokine secretion by exhausting T cells from the blood of AE patients ex vivo. However, several studies have shown that anti-PD-L1 or combined with albendazole treatment potently inhibited E. multilocularis growth in an intraperitoneal (secondary) or oral (primary) infection mouse model at early (0–4 weeks) or later (6–14 weeks) stages. This effect was associated with increased effector T-cell function and decreased regulatory T-cell (Treg)/helper T-cell (Th2) responses11,12. Recent studies on cancer, viral and parasitic infections have also reported better activity for anti-PD-1 given early in the disease course25,38,39. These and our present data suggest that the timing of blockade relative to infection (early versus later) is likely a key factor in determining whether PD-1 blockade will be beneficial versus detrimental in any given infection or cancer setting40. For example, in a tumour model, early anti-PD-1 treatment elicited robust antitumour immunity by enhancing T-cell tumour infiltration, whereas treatment of late-stage tumours in the same model was ineffective and associated with infiltration of G-MDSCs that correlated with a lack of response to anti-PD-1 therapy25. PD-1 blockade may exert different effects depending on the degree of T-cell exhaustion. Our results showed that liver CD4+ T cells and CD8+ T cells harvested from infected mice at the late stage (24 weeks) exhibited a higher level of PD-1 expression than those harvested from mice at the early and middle stages of infection (2 and 12 weeks). Several studies have also demonstrated that the effector function of T cells expressing intermediate levels of PD-1 can be restored by PD-1 blockade, while the function of T cells expressing high levels of PD-1 cannot be restored3,7,41. A smaller tumour burden usually indicates a better therapeutic response to immune checkpoint inhibitor treatment and longer overall or progression-free survival4,5,42,43,44. Hence, the results of our parasitic model suggest that high metacestode burden and PD-1 expression level at later stages might be associated with an immunosuppressive microenvironment around liver lesions, which determines the low efficacy of anti-PD-1/anti-PD-L1 treatment.
Our findings of resistance to checkpoint blockade may also be related to differences in the sites of lesions (i.e., liver versus peritoneum). Interestingly, data from previous reports and this study revealed that blocking the PD-1 pathway restores the effector function of intraperitoneal T cells infiltrating peritoneal lesions but not that of local T cells harvested from the liver after natural infection11,12. Importantly, we found that local T cells taken from the liver exhibited higher PD-1 expression than those taken from the periphery (i.e., PBMCs or spleen) in AE patients as well as in a mouse model at the late stage of infection, suggesting that the cells present within the chronic inflammatory hepatic microenvironment may be more ‘exhausted’ than those circulating in the periphery and/or subjected to more ‘exhausting’ influences from other cell types, such as G-MDSCs7,41. These data indicate that differences in local immune characteristics and the organ microenvironment are important factors to consider when predicting responsiveness to PD-1 blockade therapy, suggesting that organ-specific strategies are important for treating organ-specific diseases. These results support the need to better define populations of T cells at late stages of chronic infection or in tumours when considering the impact that PD-1 blockade could have on the course of infection or cancer45,46. The particular ‘tolerogenic’ functions of cell populations that reside in the liver have long been emphasised47. Supporting the particularities of the hepatic immunological microenvironment, we found that at the parasitic site of lesions in the liver, a subset of highly PD-1-expressing CD4+ T cells and CD8+ T cells displayed a tissue-resident memory (Trm) cell phenotype characterised by the expression of typical surface markers (i.e., CD44 and CD69) in mice. These cells stably reside in tissues and play a critical role in local immunosurveillance or in restraining immunopathology48,49. PD-1 expression was found to be elevated on Trm cells localised at the target sites of different chronic inflammatory diseases or tumours, displaying more signs of exhaustion than recirculating memory T cells50,51. Furthermore, other key factors (e.g., MDSCs) in the inflammatory hepatic microenvironment can promote T-cell exhaustion locally and contribute to anti-PD-1/anti-PD-L1 resistance in tumours as well as infectious diseases52,53,54. Our enrichment analysis also highlighted the role of myeloid leukocyte migration, differentiation and activation, which are related to the characteristics, recruitment and immunosuppressive function of myeloid cells (i.e., MDSCs) in the livers of AE patients.
One of the major characteristics of MDSCs is their ability to inhibit the immune response of T cells55,56,57. Here, we found that targeting MDSCs with anti-Gr-1 alone induced T-cell immune activation and moderately delayed the growth of metacestode; furthermore, targeting PD-1 and MDSCs together was superior to either single-agent treatment, and effectively improved the efficacy of PD-1 deficiency or PD-1 blockade therapy in our experimental model. As a result, the combined treatment increased the proportion of liver-infiltrating T cells producing IFN-γ (but not TNF-α and IL-2) significantly more than anti-Gr-1 alone (Fig. 7f), providing a major source of IFN-γ that confers host protection during chronic infection. Increased production of IFN-γ is a marker for the transition from a T exhaustive phenotype to a T effector cell phenotype58. In addition, a robust immune response by IFN-γ-producing T cells is necessary to control parasite replication and/or growth in a number of parasitic infections, and loss of this cytokine also leads to a loss of these protective mechanisms59. Our and others’ studies have demonstrated that IFN-γ production is critical for preventing disease progression in chronic E. multilocularis model and AE patients60,61,62,63. In addition, our data suggest that G-MDSCs could play a major role in the resistance to checkpoint blockade we observed and, more generally, in the immunosuppression of T cells and in the chronic characteristics of E. multilocularis infection. Similarly, a study in late Mesocestoides vogae infection demonstrated that the accumulation of G-MDSCs had greater suppressive effects than M-MDSCs64. There were a few reports of MDSCs which expand and suppress immune responses in Schistosoma, Leishmania donovani, and Toxoplasma gondii (T. gondii) infections65,66,67,68,69,70, and a significant increase in MDSCs and their role in inhibiting the differentiation and activity of T helper 2 cells in a NO-dependent manner has been shown during persistent infection with E. granulosus27,28. The presence of MDSCs may be one of the main contributors to the immunosuppressive liver microenvironment; MDSCs were shown to correlate with decreased efficacy of immune checkpoint therapy (e.g., anti-PD-1/anti-PD-L1) in colorectal cancer53.
Previous work also demonstrated that MDSCs exert their antagonistic effect on T cells by depleting amino acids via arginase 1 (ARG1) and 2 (ARG2) and IDO1, or by upregulating INOS and inhibitory cytokines (e.g., IL-10)21,56,71,72. In our study, the expression levels of IDO1 and INOS, rather than ARG1/2, were significantly increased in the livers of AE patients, and IDO1 expression was colocalized with CD33+ cells in the livers of AE patients. IDO+ MDSCs were also increased in the livers of PD-1-deficient infected mice. The expression level of IDO1, rather than that of INOS or IL-10, in the periphrastic area of the liver in AE patients was positively correlated with lesion metabolic activity according to PET-CT. Some studies have shown that the lack of INOS expression by peritoneal and splenic macrophages rather than MDSCs, confers a certain degree of resistance against persistent chronic infection with E. multilocularis73,74; moreover, no IL-10 was detected when polymorphonuclear granulocytes (PMN, the phenotype of which overlaps with G-MDSCs75) from AE patients were cultured with metacestode vesicles76,77,78. In addition, elevated IDO1 expression promotes immunosuppression and AE progression by inhibiting the activation, clonal expansion and differentiation of T cells79. Similarly, E. granulosus antigens (e.g., recombinant Eg10, EgB, mMDH) can upregulate IDO1 expression to induce host immune tolerance and promote chronic infection80,81. We also showed that inhibition of IDO1 by 1-MT significantly attenuated MDSC-mediated suppression of T-cell function and enhanced IFN-γ and TNF-α secretion by T cells in vitro. This finding strongly suggested that the immunosuppressive activity of MDSCs in E. multilocularis infection is IDO1-dependent and leads to anti-PD-1 resistance. Future experiments will evaluate the therapeutic significance of combining IDO1-specific inhibitors with immune checkpoint blockade to prevent disease progression during persistent parasitic infection. High expression of IDO in dendritic cells reportedly increases Leishmania spp. infection and facilitates pathogen survival as well82,83. The inhibition of increased IDO activity was shown to be involved in antiparasitic mechanisms during T. gondii infection84. Overexpression of IDO1 also facilitates T-cell anergy in noninfectious disease models85,86.
In summary, our study demonstrated that the resistance to anti-PD-1 checkpoint interventions observed in chronic E. multilocularis infection is mainly attributed to the accumulation of G-MDSCs around liver lesions and their substantial inhibitory effects on T-cell immune function, in part via an alternative IDO1-dependent mechanism. The removal of G-MDSC-mediated immunosuppression by anti-Gr-1 antibody administration can effectively restore T-cell function and potentiate PD-1 blockade therapy. These findings provide additional support for the mechanisms of T-cell exhaustion through checkpoint inhibition associated with G-MDSC IDO1-dependent immune suppression, as suggested in other models, both in cancer and in other types of chronic infection. In addition, they provide preclinical evidence in support of targeting MDSC or combining such an approach with the check-point blockade in patients with advanced AE, a severe disease with only limited treatment options.
Methods
Ethics statement
This study protocol was approved by the ethics committee of the First Affiliated Hospital of Xinjiang Medical University (N° S20130418-3), and all patients provided informed written consent in accordance with the Declaration of Helsinki (1975) of the World Medical Association. All the data of the human subjects are summarised in Supplementary Data 2.
Human donors
Liver specimens were obtained from 64 patients with AE who underwent liver resection. Patients with immune suppression-associated conditions, as described by Chauchet et al. 16, were excluded. AE diagnosis was confirmed in all patients by liver biopsies. One specimen was taken close to the parasitic lesion, including the metacestode (CLT, ‘close liver tissue’, ~ 0.5 cm from lesion), and/or one was taken from the macroscopically normal liver distant from the lesion (DLT, ‘distant liver tissue’, at least 2 cm distant from lesion), as described in our previous publication9. Peripheral blood samples (PB) were obtained from 33 AE patients and from 34 healthy age- and sex-matched controls. The number of liver and blood samples, types of measurements, and purpose of comparisons are given in Supplementary Data 1.
Liver pathology and immunohistochemistry
Liver tissue samples were fixed in 4% paraformaldehyde (PFA)/PBS for 48 hr. Dehydrated, paraffin-embedded liver tissues were cut into 5- μm sections, which were then processed for pathological evaluation or immunohistochemistry. The sections were subjected to staining and microscopically examined, and photographs were taken using a digital image-capture system (Olympus, Tokyo, Japan).
For pathological analysis, sections were stained with haematoxylin and eosin (H&E) to evaluate infiltrating cells and liver immune microenvironment formation according to guidelines for clinical samples.
For immunohistochemistry analysis, the sections were deparaffinized and then subjected to heat-mediated antigen-retrieval in Tris-EDTA buffer (Solarbio, Beijing, China). The sections were blocked for 1 hr at room temperature in PBS with 10% goat serum (blocking buffer) and then incubated at 4 °C overnight with primary antibodies in blocking buffer (anti-human CD33, 1:100, Abcam; anti-human IDO1, 1:500, Abcam; anti-human INOS, 1:75, Abcam, Cambridge, UK). The next day, the sections were washed three times for 5 min and incubated for 2 hr at room temperature with a secondary antibody (goat anti-rabbit F(ab’)2-HRP, Abcam, Cambridge, UK). Staining was developed using a 3, 3’ diaminobenzidine (DAB) substrate kit (Abcam, Cambridge, UK) according to the manufacturer’s instructions. A total of 3-5 fields/sections/samples were assessed at × 400 magnification using cellSens Dimension software (Olympus, Japan) for computerised quantification, and the results are expressed as the intensity of positive staining per field.
Immunofluorescence
For immunofluorescence analysis, the frozen sections of liver tissue were stained with primary antibodies (anti-human CD4, 1:250, Abcam; anti-human CD8, 1:250, Abcam; anti-PD-1, 1:200, Abcam; anti-human CD33, 1:200, Abcam; anti-human IDO1, 1:500, Abcam, Cambridge, UK) at 4 °C in blocking buffer overnight and subsequently stained with secondary antibodies (Alexa Fluor® 488-labelled anti-rat IgG, Cell Signalling Technology; Alexa Fluor® 488-labelled anti-mouse IgG, Cell Signalling Technology; Alexa Fluor® 555-labelled anti-mouse IgG, Cell Signalling Technology, Boston, United States) for 2 hr at room temperature. 4’, 6-Diamidino-2-phenylindole (DAPI) was used for nuclear staining. Images were acquired by a confocal laser scanning fluorescence microscope (Leica, Oskar-Barnack-Straße). Positive cells were quantified by ImagePro Plus software (Media Cybernetics, Rockville, United States) and are expressed as the mean number of positive cells in five fields at 200 × magnification.
Isolation of mononuclear cells from human liver tissues
Close- and distant-liver tissue-infiltrating cells were obtained from paired fresh liver tissue samples of AE patients as previously described87. For isolation of liver mononuclear cells, liver tissue was cut into small pieces and digested in RPMI 1640 supplemented with 0.05% collagenase IV (Sigma-Aldrich), 0.02% DNase I (Roche, Basel), and 20% FBS (HyClone) at 37 °C for 1 h. Dissociated cells were filtered through a 150 µm mesh and separated by Ficoll (Solarbio, Beijing, China) centrifugation, and the mononuclear cells were washed and resuspended in RPMI 1640 supplemented with 10% FBS.
Isolation of mononuclear cells from human peripheral blood
Peripheral blood mononuclear cells (PBMCs) were purified from blood samples by Ficoll (Solarbio, Beijing, China) density gradient centrifugation as previously described88. In brief, 6–8 mL blood prediluted 1:1 in PBS was carefully added to 3 ml of Ficoll liquid in a 15 mL tube and then was centrifuged at 400 × g for 30 min at 25–27 °C. PBMCs were washed and resuspended in RPMI 1640 supplemented with 10% FBS.
Flow cytometry
A single-cell suspension of leukocytes from human samples was resuspended in RPMI 1640 containing 10% FBS, 1000 mg/mL penicillin and 1000 µ/mL streptomycin (HyClone, Beijing, China). For cell surface staining, 0.5 × 106 cells per tube were stained for surface markers using antibodies for 30 min at 4 °C in the dark. For intracellular staining, 1 × 106 cells per tube were cultured in the presence of Cell Stimulation Cocktail (eBioscience, San Diego, United States), according to the manufacturer’s instructions and incubated at 37 °C for 4 h. The cells were first stained for surface markers using antibodies for 30 min at 4 °C in the dark. The cells were then suspended in a permeabilization buffer containing antibodies according to the manufacturer’s instructions (BioLegend, San Diego, United States). The antibodies used herein are listed in Supplementary Data 3. An LSRFortessa flow cytometer (BD Immunocytometry Systems, San Diego, United States) was used to acquire the data, which were analysed with the FlowJo software 7.6.1 (Treestar, San Carlos, United States).
A single-cell suspension of mononuclear cells from mouse samples was incubated in PBS (0.2% BSA and 0.1% sodium azide) in the presence of neutralising monoclonal antibodies against CD16:CD32 (Fc Block; Biolegend, San Diego, United States) for 20 min at 4 °C prior to staining. For cell surface staining, 0.5 × 106 cells per tube were stained for surface markers using specific antibodies in PBS buffer for 30 min at 4 °C in the dark. The following phenotypes were used to determine the MDSC populations: CD45+CD11b+Gr-1+ for MDSCs; CD45+CD11b+Gr-1+Ly6Clow for G-MDSCs; and CD45+CD11b+Gr-1+Ly6C+ for M-MDSCs89,90. The protocol for intracellular staining was the same as that described above. The antibodies used herein are listed in Supplementary Data 3. The samples were then analysed using an LSRFortessa flow cytometer and the FlowJo software 7.6.1 (Treestar, San Carlos, United States).
Ex vivo T-cell function antibody blockade
PBMCs were isolated from AE patients and restimulated with anti-human CD3 (2.5 μg/ml, BD Biosciences) and anti-human CD28 (1.25 μg/ml, BD Biosciences) at 37 °C in the presence of anti-human PD-1 mAb (5 µg/ml, R&D Systems) or isotype control (R&D Systems). After 20 h of incubation and 6 h of brefeldin A (1000 dilution, BD Biosciences), the cells were harvested to determine the intracellular cytokine production (IFN-γ and TNF-α) of CD4+ T cells and CD8+ T cells using flow cytometry.
Mice
Wild-type (WT) female C57BL/6 (B6) and BALB/c mice were purchased from Beijing Vital River Experimental Animal Technology Co., Ltd. PD-1-/- mice, which were originally generated by Dr. Tasuku Honjo (Kyoto University, Kyoto, Japan), were kindly provided by Dr. Yuzhang Wu (Army Medical University, Chongqing, China). All mice were maintained under specific pathogen-free conditions according to the guidelines for experimental animals established by the Animal Care and Use Committee and the Ethical Committee of the First Affiliated Hospital of Xinjiang Medical University (N° 20140411-05).
Mouse model of E. multilocularis infection and in vivo blockade
Mice were inoculated via the hepatic portal vein with live protoscoleces (PSCs) in saline as previously described8, whereas control mice were injected with isotonic saline.
At necropsy, the whole weight of the liver was measured using an electronic scale; metacestode tissue was carefully removed from the liver lobes by using microsurgery forceps and scalpel blades. The metacestode tissue, which was free of host tissue, was immediately weighed on an electronic scale. The formation of all parasitic foci was observed on haematoxylin and eosin (H&E)-stained sections and the number of infectious foci with metacestode structures (the confluent lesions) was counted in all liver lobes as previously described8.
For in vivo blockade, mice bearing metacestodes of 1.5–3 mm2 after 12 weeks were randomised into treatment groups and treated with anti-PD-1 mAb (200 μg, clone RMP1-14, BioXcell, West Lebanon, USA), anti-PD-L1 mAb (200 μg, clone 10 F.2H11, BioXcell), or isotype-control antibody (mouse IgG1, clone 2A3 or LTF-2, BioXcell) by intraperitoneal (i.p.) injection two or three times per week for 12 weeks. For depletion of MDSCs, mice were injected with 200 μg of anti-Ly6G/Ly6C (Gr-1) mAb (clone RB6-8C5, BioXcell) or isotype control antibody (clone LTF-2, BioXcell) i.p. two times per week for 12 weeks. For treatment experiments with a combination of anti-PD-1 mAb and anti-Ly6G/Ly6C (Gr-1) mAb, mice were intraperitoneally injected. According to the above dose and time points, control mice received both control isotypes.
Isolation of mononuclear cells from mouse liver and spleen
A single-cell suspension of mononuclear cells was isolated from the liver and spleen as described previously. Livers were homogenised and mononuclear cells were separated from hepatocytes by centrifugation with 40% Percoll (GE Healthcare, Pittsburgh, United States). The spleens were crushed between two glass slides, suspended in PBS containing 0.2% BSA, and passed through a 74 μm nylon mesh. Red blood cells were depleted using red blood lysis buffer (BioLegend, San Diego, United States). The cells were then manually counted on a haemocytometer.
In vitro coculture of T cells and G-MDSCs
Splenic CD4+ T cells or CD8+ T cells were enriched from PD-1-/- mice by positive magnetic selection (Miltenyi, Germany). Splenic G-MDSCs were enriched from E. multilocularis-infected mice by positive magnetic selection (Miltenyi, Germany). Purified CD4+ or CD8+ T cells (5 × 105/ml) were cocultured with G-MDSCs (105/ml) for 48 h in the presence of anti-mouse CD3 (2.5 μg/ml, eBiosciences) and anti-mouse CD28 (1.25 μg/ml, eBiosciences). The IDO1 inhibitor 1-MT (5 μg/ml, Sigma-Aldrich®, United States) or medium alone was added to the culture. Coculture supernatants were collected for IFN-γ and TNF-α analysis by enzyme-linked immunosorbent assays (ELISA).
Enzyme-linked immunosorbent assays (ELISAs)
The culture supernatants were used for the measurement of IFN-γ and TNF-α. The concentrations of cytokines were measured using ELISA kits according to the manufacturer’s instructions (Thermo Fisher Scientific).
Quantitative reverse transcription-PCR (qRT-PCR) assays
Total RNA was extracted from liver tissue using TRIzol Reagent (Invitrogen, Carlsbad, CA) according to the manufacturer’s instructions. M-MLV Transcriptase was used for reverse transcription according to the manufacturer’s instructions (Thermo Fisher Scientific, Waltham, MA). qRT-PCR was performed in a thermocycler (iQ5 Bio-Rad, Hercules, CA) with the SYBR Green PCR premix (TaKaRa, Dalian) according to the manufacturer’s protocol. The PCR primers used herein are listed in Supplementary Data 3. The results were normalised with respect to the value obtained for the housekeeping gene GAPDH. The △Ct was calculated by subtracting the Ct value of the housekeeping gene (GAPDH) from that of the target gene △Ct. The △△Ct was calculated by subtracting the △Ct of the experimental group target gene from the △Ct of the control group target gene. Relative mRNA expression was calculated by the 2−△△Ct method.
Data analysis
Single-cell sequences for 4 AE patients were retrieved from a public database (accession no. HRA000553) reported in our previous study91. Hepatic mRNA expression profiles for 6 AE patients were retrieved from the GEO database (GSE124362) reported in our previous study9. Gene set enrichment analysis (GSEA) was performed using the Broad Institute tool GSEA v.2.2.1. In addition, hierarchical clustering of genes and arrays was performed using the R software heatmap package.
Statistical analysis
Student’s t test was used to compare two groups, and one-way analysis of variance (ANOVA) was used to compare three or more groups. Pearson’s correlation was used to calculate the strength of a relationship. All the data are presented as the mean ± standard deviation (SD). p < 0.05 was considered to indicate statistical significance.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The RNA sequencing data in this study are available in the figshare database under accession code HRA000553 (https://figshare.com/s/f2a4578be27c2cb767f9). The mRNA expression data in this study are available in the Gene Expression Omnibus database under accession code GSE124362 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc= GSE124362). The key reagents or resources used in this study are listed in Supplementary Data 3. Source data are provided with this paper.
Code availability
The data analysis pipeline in our study is described on the Seurat official website and clusterProfiler official website. The code can be found in Supplementary Data 4.
Change history
27 August 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41467-024-51832-6
References
Philip, M. & Schietinger, A. Heterogeneity and fate choice: T cell exhaustion in cancer and chronic infections. Curr. Opin. Immunol. 58, 98–103 (2019).
Blank, C. U. et al. Defining ‘T cell exhaustion’. Nat. Rev. Immunol. 19, 665–674 (2019).
LaFleur, M. W., Muroyama, Y., Drake, C. G. & Sharpe, A. H. Inhibitors of the PD-1 pathway in tumor therapy. J. Immunol. 200, 375–383 (2018).
Hopkins, A. M., Kichenadasse, G., McKinnon, R. A., Rowland, A. & Sorich, M. J. Baseline tumor size and survival outcomes in lung cancer patients treated with immune checkpoint inhibitors. Semin. Oncol. 46, 380–384 (2019).
Nishino, M., Giobbie-Hurder, A., Ramaiya, N. H. & Hodi, F. S. Response assessment in metastatic melanoma treated with ipilimumab and bevacizumab: CT tumor size and density as markers for response and outcome. J. Immunother. Cancer 2, 40 (2014).
Sharma, P., Hu-Lieskovan, S., Wargo, J. A. & Ribas, A. Primary, adaptive, and acquired resistance to cancer immunotherapy. Cell 168, 707–723 (2017).
Jubel, J. M., Barbati, Z. R., Burger, C., Wirtz, D. C. & Schildberg, F. A. The role of PD-1 in acute and chronic infection. Front. Immunol. 11, 487 (2020).
Zhang, C. et al. T-cell tolerance and exhaustion in the clearance of Echinococcus multilocularis: role of inoculum size in a quantitative hepatic experimental model. Sci. Rep. 7, 11153 (2017).
Zhang, C. et al. Immune exhaustion of T cells in alveolar echinococcosis patients and its reversal by blocking checkpoint receptor TIGIT in a murine model. Hepatology 71, 1297–1315 (2020).
Li, D. et al. Upregulation of LAG3 modulates the immune imbalance of CD4+ T-cell subsets and exacerbates disease progression in patients with alveolar echinococcosis and a mouse model. PLoS Pathog. 19, e1011396 (2023).
Jebbawi, F. et al. Innate and adaptive immune responses following PD-L1 blockade in treating chronic murine alveolar echinococcosis. Parasite Immunol. 43, e12834 (2021).
Wang, J. et al. Immunotherapy of alveolar echinococcosis via PD-1/PD-L1 immune checkpoint blockade in mice. Parasite Immunol. 40, e12596 (2018).
Wen, H. et al. Echinococcosis: Advances in the 21st Century. Clin. Microbiol. Rev. 32, e00075 (2019).
Autier, B. et al. Alveolar echinococcosis in immunocompromised hosts. Clin. Microbiol. Infect. 29, 593–599 (2023).
Manfras, B. J., Reuter, S., Wendland, T. & Kern, P. Increased activation and oligoclonality of peripheral CD8(+) T cells in the chronic human helminth infection alveolar echinococcosis. Infect. immun. 70, 1168–1174 (2002).
Chauchet, A. et al. Increased incidence and characteristics of alveolar echinococcosis in patients with immunosuppression-associated conditions. Clin. Infect. Dis. 59, 1095–1104 (2014).
Umansky, V., Blattner, C., Gebhardt, C. & Utikal, J. The role of myeloid-derived suppressor cells (MDSC) in cancer progression. Vaccines 4, 36 (2016).
Bronte, V. & Zanovello, P. Regulation of immune responses by L-arginine metabolism. Nat. Rev. Immunol. 5, 641–654 (2005).
Rodriguez, P. C. & Ochoa, A. C. Arginine regulation by myeloid derived suppressor cells and tolerance in cancer: mechanisms and therapeutic perspectives. Immunol. Rev. 222, 180–191 (2008).
Onyilagha, C., Kuriakose, S., Ikeogu, N., Jia, P. & Uzonna, J. Myeloid-derived suppressor cells Contribute to susceptibility to trypanosoma congolense infection by suppressing CD4(+) T cell proliferation and IFN-gamma production. J. Immunol. 201, 507–515 (2018).
Yu, J. et al. Myeloid-derived suppressor cells suppress antitumor immune responses through IDO expression and correlate with lymph node metastasis in patients with breast cancer. J. Immunol. 190, 3783–3797 (2013).
Veglia, F., Perego, M. & Gabrilovich, D. Myeloid-derived suppressor cells coming of age. Nat. Immunol. 19, 108–119 (2018).
Highfill, S. L. et al. Disruption of CXCR2-mediated MDSC tumor trafficking enhances anti-PD1 efficacy. Sci. Transl. Med. 6, 237ra267 (2014).
Bao, Y. et al. Targeting m(6)A reader YTHDF1 augments antitumour immunity and boosts anti-PD-1 efficacy in colorectal cancer. Gut 72, 1497–1509 (2023).
Kim, W. et al. PD-1 Signaling promotes tumor-infiltrating myeloid-derived suppressor cells and gastric tumorigenesis in mice. Gastroenterology 160, 781–796 (2021).
Stevenson, M. M., Valanparambil, R. M. & Tam, M. Myeloid-derived suppressor cells: The expanding world of helminth modulation of the immune system. Front. Immunol. 13, 874308 (2022).
Pan, W. et al. Surveillance on the status of immune cells after Echinnococcus granulosus protoscoleces infection in Balb/c mice. PloS ONE 8, e59746 (2013).
Zhou, X. et al. Myeloid-derived suppressor cells exert immunosuppressive function on the T helper 2 in mice infected with Echinococcus granulosus. Exp. Parasitol. 215, 107917 (2020).
Ahmed, R. & Gray, D. Immunological memory and protective immunity: understanding their relation. Science 272, 54–60 (1996).
Zaph, C. et al. Persistence and function of central and effector memory CD4+ T cells following infection with a gastrointestinal helminth. J. Immunol. 177, 511–518 (2006).
Krzych, U., Zarling, S. & Pichugin, A. Memory T cells maintain protracted protection against malaria. Immunol. Lett. 161, 189–195 (2014).
Harty, J. T., Tvinnereim, A. R. & White, D. W. CD8+ T cell effector mechanisms in resistance to infection. Annu. Rev. Immunol. 18, 275–308 (2000).
Pauken, K. E. & Wherry, E. J. Overcoming T cell exhaustion in infection and cancer. Trends Immunol. 36, 265–276 (2015).
Lu, L. et al. Loss of natural resistance to schistosome in T cell deficient rat. PLoS Negl. Trop. Dis. 14, e0008909 (2020).
La, X. et al. Upregulation of PD-1 on CD4(+)CD25(+) T cells is associated with immunosuppression in liver of mice infected with Echinococcus multilocularis. Int. Immunopharmacol. 26, 357–366 (2015).
Li, Y. et al. Role of soluble programmed death-1 (sPD-1) and sPD-ligand 1 in patients with cystic echinococcosis. Exp. Ther. Med. 11, 251–256 (2016).
Ben Salah, E. et al. Soluble programmed death-1 (sPD-1) as predictor of early surgical outcomes of paediatric cystic echinococcosis. Parasite Immunol. 43, e12809 (2021).
Ribas, A. et al. Association of pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA 315, 1600–1609 (2016).
Markowitz, G. J. et al. Immune reprogramming via PD-1 inhibition enhances early-stage lung cancer survival. JCI Insight 3, e96836 (2018).
Kauffman, K. D. et al. PD-1 blockade exacerbates Mycobacterium tuberculosis infection in rhesus macaques. Sci. Immunol. 6, eabf3861 (2021).
Nakamoto, N. et al. Functional restoration of HCV-specific CD8 T cells by PD-1 blockade is defined by PD-1 expression and compartmentalization. Gastroenterology 134, 1927–1937 (2008).
Chardin, D. et al. Baseline metabolic tumor volume as a strong predictive and prognostic biomarker in patients with non-small cell lung cancer treated with PD1 inhibitors: a prospective study. J. Immunother. Cancer 8, e000645 (2020).
Joseph, R. W. et al. Baseline tumor size is an independent prognostic factor for overall survival in patients with melanoma treated with pembrolizumab. Clin. Cancer Res. 24, 4960–4967 (2018).
Wen, Z. et al. High baseline tumor burden-associated macrophages promote an immunosuppressive microenvironment and reduce the efficacy of immune checkpoint inhibitors through the IGFBP2-STAT3-PD-L1 pathway. Cancer Commun. 43, 562–581 (2023).
Caraballo Cortes, K. et al. Expression of programmed cell death protein 1 and T-cell immunoglobulin- and mucin-___domain-containing molecule-3 on peripheral blood CD4+CD8+ double positive T cells in patients with chronic hepatitis C virus infection and in subjects who spontaneously cleared the virus. J. Viral Hepat. 26, 942–950 (2019).
Pandey, A., Ezemenari, S., Liaukovich, M., Richard, I. & Boris, A. A rare case of pembrolizumab-induced reactivation of hepatitis B. Case Rep. Oncol. Med. 2018, 5985131 (2018).
Robinson, M. W., Harmon, C. & O’Farrelly, C. Liver immunology and its role in inflammation and homeostasis. Cell. Mol. Immunol. 13, 267–276 (2016).
Petrelli, A. et al. PD-1+CD8+ T cells are clonally expanding effectors in human chronic inflammation. J. Clin.Invest. 128, 4669–4681 (2018).
Shwetank et al. Maintenance of PD-1 on brain-resident memory CD8 T cells is antigen independent. Immunol. Cell Biol. 95, 953–959 (2017).
Gitto, S., Natalini, A., Antonangeli, F. & Di Rosa, F. The Emerging Interplay Between Recirculating and Tissue-Resident Memory T Cells in Cancer. Front. Immunol. 12, 755304 (2021).
Mami-Chouaib, F. et al. Resident memory T cells, critical components in tumor immunology. J. Immunother. Cancer 6, 87 (2018).
Zhang, Q. Q. et al. CD11b deficiency suppresses intestinal tumor growth by reducing myeloid cell recruitment. Sci. Rep. 5, 15948 (2015).
Abushukair, H., Ababneh, O., Zaitoun, S. & Saeed, A. Primary and secondary immune checkpoint inhibitors resistance in colorectal cancer: Key mechanisms and ways to overcome resistance. Cancer Treat. Res. Commun. 33, 100643 (2022).
Wei, C. Y. et al. PKCalpha/ZFP64/CSF1 axis resets the tumor microenvironment and fuels anti-PD1 resistance in hepatocellular carcinoma. J. Hepatol. 77, 163–176 (2022).
Kusmartsev, S. A., Li, Y. & Chen, S. H. Gr-1+ myeloid cells derived from tumor-bearing mice inhibit primary T cell activation induced through CD3/CD28 costimulation. J. Immunol. 165, 779–785 (2000).
Srivastava, M. K., Sinha, P., Clements, V. K., Rodriguez, P. & Ostrand-Rosenberg, S. Myeloid-derived suppressor cells inhibit T-cell activation by depleting cystine and cysteine. Cancer Res. 70, 68–77 (2010).
Preite, N. W., Kaminski, V. L., Borges, B. M., Calich, V. L. G. & Loures, F. V. Myeloid-derived suppressor cells are associated with impaired Th1 and Th17 responses and severe pulmonary paracoccidioidomycosis which is reversed by anti-Gr1 therapy. Front. Immunol. 14, 1039244 (2023).
Ajith, A. et al. Targeting TREM1 augments antitumor T cell immunity by inhibiting myeloid-derived suppressor cells and restraining anti-PD-1 resistance. J. Clin. Invest. 133, e167951 (2023).
Marinho, C. R. et al. IFN-gamma, but not nitric oxide or specific IgG, is essential for the in vivo control of low-virulence Sylvio X10/4 Trypanosoma cruzi parasites. Scand. J. Immunol. 66, 297–308 (2007).
Schmid, M. et al. Use of interferon gamma and mebendazole to stop the progression of alveolar hydatid disease: case report. Clin. Infect. Dis. 20, 1543–1546 (1995).
Jenne, L., Kilwinski, J., Radloff, P., Flick, W. & Kern, P. Clinical efficacy of and immunologic alterations caused by interferon gamma therapy for alveolar echinococcosis. Clin. Infect. Dis. 26, 492–494 (1998).
Liance, M., Ricard-Blum, S., Emery, I., Houin, R. & Vuitton, D. A. Echinococcus multilocularis infection in mice: in vivo treatment with a low dose of IFN-gamma decreases metacestode growth and liver fibrogenesis. Parasite 5, 231–237 (1998).
Zhang, C. et al. Involvement of TIGIT in natural killer cell exhaustion and immune escape in patients and mouse model with liver echinococcus multilocularis infection. Hepatology 74, 3376–3393 (2021).
Macak Kubaskova, T., Mudronova, D., Vargova, M., Reiterova, K. & Hrckova, G. Cellular and humoral peritoneal immunity to Mesocestoides vogae metacestode infection in mice. Parasites & vectors 14, 54 (2021).
Zhang, Y. et al. Granulocytic myeloid-derived suppressor cells inhibit T follicular helper cells during experimental Schistosoma japonicum infection. Parasit. Vectors 14, 497 (2021).
Yang, Q. et al. A schistosoma japonicum infection promotes the expansion of myeloid-derived suppressor cells by activating the JAK/STAT3 pathway. J. Immunol. 198, 4716–4727 (2017).
Bandyopadhyay, S. et al. Glycyrrhizic acid-mediated subdual of myeloid-derived suppressor cells induces antileishmanial immune responses in a susceptible host. Infect. Immun. 83, 4476–4486 (2015).
Pereira, W. F. et al. Myeloid-derived suppressor cells help protective immunity to Leishmania major infection despite suppressed T cell responses. J. Leukoc. Biol. 90, 1191–1197 (2011).
Qi, H. et al. Tim-3 regulates the immunosuppressive function of decidual MDSCs via the Fyn-STAT3-C/EBPbeta pathway during Toxoplasma gondii infection. PLoS Pathog. 19, e1011329 (2023).
Bahwal, S. A. et al. Attenuated Toxoplasma gondii enhances the antitumor efficacy of anti-PD1 antibody by altering the tumor microenvironment in a pancreatic cancer mouse model. J. Cancer Res. Clin. Oncol. 148, 2743–2757 (2022).
Pan, P. Y. et al. Immune stimulatory receptor CD40 is required for T-cell suppression and T regulatory cell activation mediated by myeloid-derived suppressor cells in cancer. Cancer Res. 70, 99–108 (2010).
Corzo, C. A. et al. Mechanism regulating reactive oxygen species in tumor-induced myeloid-derived suppressor cells. J. Immunol. 182, 5693–5701 (2009).
Dai, W. J., Waldvogel, A., Jungi, T., Stettler, M. & Gottstein, B. Inducible nitric oxide synthase deficiency in mice increases resistance to chronic infection with Echinococcus multilocularis. Immunology 108, 238–244 (2003).
Dai, W. J. & Gottstein, B. Nitric oxide-mediated immunosuppression following murine Echinococcus multilocularis infection. Immunology 97, 107–116 (1999).
Hegde, S., Leader, A. M. & Merad, M. MDSC: Markers, development, states, and unaddressed complexity. Immunity 54, 875–884 (2021).
Dreweck, C. M., Soboslay, P. T., Schulz-Key, H., Gottstein, B. & Kern, P. Cytokine and chemokine secretion by human peripheral blood cells in response to viable Echinococcus multilocularis metacestode vesicles. Parasite Immunol. 21, 433–438 (1999).
Eger, A. et al. Pro-inflammatory (IL-1beta, IL-18) cytokines and IL-8 chemokine release by PBMC in response to Echinococcus multilocularis metacestode vesicles. Parasite Immunol. 25, 103–105 (2003).
Margos, M. C., Grandgirard, D., Leib, S. & Gottstein, B. In vitro induction of lymph node cell proliferation by mouse bone marrow dendritic cells following stimulation with different Echinococcus multilocularis antigens. J Helminthol 85, 128–137 (2011).
Meng, R. et al. Indoleamine 2,3-dioxygenase 1 signaling orchestrates immune tolerance in Echinococcus multilocularis-infected mice. Front. Immunol. 13, 1032280 (2022).
Wang, Y. et al. Mechanisms underlying immune tolerance caused by recombinant Echinococcus granulosus antigens Eg mMDH and Eg10 in dendritic cells. PloS ONE 13, e0204868 (2018).
Shan, J. Y. et al. [Echinococcus granulosus recombinant antigen B induced IDO expression in mouse bone marrow-derived dendritic cells in vitro]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 29, 111–116 (2011).
Makala, L. H. et al. Leishmania major attenuates host immunity by stimulating local indoleamine 2,3-dioxygenase expression. J. Infect. Dis. 203, 715–725 (2011).
Makala, L. H. The role of indoleamine 2, 3 dioxygenase in regulating host immunity to leishmania infection. J. Biomed. Sci. 19, 5 (2012).
Murakami, Y. et al. Inhibition of increased indoleamine 2,3-dioxygenase activity attenuates Toxoplasma gondii replication in the lung during acute infection. Cytokine 59, 245–251 (2012).
Tang, K., Wu, Y. H., Song, Y. & Yu, B. Indoleamine 2,3-dioxygenase 1 (IDO1) inhibitors in clinical trials for cancer immunotherapy. J. Hematol. Oncol. 14, 68 (2021).
Werfel, T. A. et al. Treatment-induced tumor cell apoptosis and secondary necrosis drive tumor progression in the residual tumor microenvironment through MerTK and IDO1. Cancer Res. 79, 171–182 (2019).
Kuang, D. M. et al. Tumor-activated monocytes promote expansion of IL-17-producing CD8+ T cells in hepatocellular carcinoma patients. J. Immunol. 185, 1544–1549 (2010).
Sun, C. et al. TGF-beta1 down-regulation of NKG2D/DAP10 and 2B4/SAP expression on human NK cells contributes to HBV persistence. PLoS Pathog. 8, e1002594 (2012).
Liao, W. et al. KRAS-IRF2 Axis drives immune suppression and immune therapy resistance in colorectal cancer. Cancer Cell 35, 559–572. e557 (2019).
Li, Y. M. et al. Receptor-interacting protein kinase 3 deficiency recruits myeloid-derived suppressor cells to hepatocellular carcinoma through the chemokine (C-X-C Motif) ligand 1-chemokine (C-X-C Motif) receptor 2 axis. Hepatology 70, 1564–1581 (2019).
Jiang, T. et al. Single-cell heterogeneity of the liver-infiltrating lymphocytes in individuals with chronic echinococcus multilocularis infection. Infect. Immun. 90, e0017722 (2022).
Acknowledgements
We thank all members of our laboratory for their support and helpful discussions, the Yuzhang Wu laboratory at Chongqing for providing PD-1-/- mice (originally generated by Dr. Tasuku Honjo, Japan), and the Lu Shi from the CRE Life Institute, Beijing. This research was supported by the National Key Research and Development Programme of China (2021YFC2300800 to CSZ, 2021YFC2300801 to CSZ, 2021YFC2300802 to CSZ), Natural Science Foundation of Xinjiang Uygur Autonomous Region (2022D01D60 to CSZ), National Natural Science Foundation of China (82160396 to CSZ, 81830066 to WBZ, 81760368 to CSZ, 82160397 to WH, 82060370 to JL), Xinjiang Uygur Autonomous Region “Tianshan Talent” Training Programme (2022TSYCCX0106 to CSZ), and Cultivation projects of the National Science Fund for Distinguished Young Scholars (xyd2021J003 to CSZ). Mice images were drawn by hand using Procreate software.
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: C.S.Z., H.W., J.L. H. Y. S and Z.G.T.; performed the experiments: C.S.Z., H.W., Z.D.L., J.L., M.L.W., Y.S.L., B.Q.D., A.D.L., X.J.K., X.R.Z., Z.B.G.R., A.B.D.A. nd Q.Y.; analysed the data: C.S.Z., H.W. and Y.S.L.; contributed to technical or materials related issues: T.E.G., Y.M.S. and W.B.Z.; draughted and revised the manuscript: C.S.Z., H. Y. S., D. A. V., H.W. and Z.G.T.; supervised the study: C.S.Z., Z.G.T. and H.W.; All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Philippe Krebs, Henry McSorley and the other anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, C., Wang, H., Aji, T. et al. Targeting myeloid-derived suppressor cells promotes antiparasitic T-cell immunity and enhances the efficacy of PD-1 blockade. Nat Commun 15, 6345 (2024). https://doi.org/10.1038/s41467-024-50754-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-50754-7
This article is cited by
-
Targeting immune checkpoints in hepatocellular carcinoma therapy: toward combination strategies with curative potential
Experimental Hematology & Oncology (2025)
-
Upregulation of CD244 promotes CD8+ T cell exhaustion in patients with alveolar echinococcosis and a murine model
Parasites & Vectors (2024)